Article:
Rhinolalia is a speech disorder manifested in distorted pronunciation of sounds associated with defects in the structure and functioning of the speech organs.
Due to the incorrect structure, at the moment of sound formation, the air stream flows in the wrong direction, which leads to distortion of the pronounced sound. This function is provided by the muscles of the palate and the walls of the pharynx, which open or close the passage into the nasal cavity.
In this case, the child’s voice may acquire a nasal quality - it seems as if he is speaking through the nose, or, if the air flows only through the mouth, the nasal sounds [m], [n] and vowels are distorted in speech - in this case they speak of a lack of nasal sound.
The consequence of rhinolalia is not only the distortion of sounds. Written speech is impaired, it is difficult for the child to master vocabulary and grammar, and psychological problems appear.
Types of rhinolalia
There is a widespread classification of rhinolalia into two types based on the reasons for its appearance: organic - when there is a violation of the structure of the speech apparatus, and functional - when there is a violation of the functioning of the speech apparatus.
When rhinolalia occurs, disturbances can be observed in the nasal or oral cavity. Therefore, there are three types of rhinolalia: open, closed and mixed.
The open form is observed when the space between the oral and nasal cavities is constantly open, when air constantly flows through the nose. This results in all spoken sounds having a nasal connotation.
The open form is most common and has three subtypes:
- Organic open rhinolalia occurs due to existing cleft palates, the absence or bifurcation of a small uvula, or a shortened soft palate.
- Organic open rhinolalia manifests itself due to the presence of paresis (incomplete paralysis) and paralysis of the soft palate.
- Functional open rhinolalia.
Closed rhinolalia occurs when there is an obstruction that blocks the space for air flow through the nose. Therefore, the pronunciation of nasal sounds [m], [n], [m], [n] and vowels suffers.
Mixed rhinolalia is a combination of the two types listed above.
If a child is diagnosed with rhinolalia, regardless of the form of manifestation of the disease, parents should immediately seek help from specialists. The most favorable treatment prognosis is given with a functional form. Closed rhinolalia requires more time and effort, which can lead to getting rid of existing speech impediments.
Sometimes they talk about rhinophony. It refers to the excess nasal tone of the voice, which occurs when there is insufficient differentiation between the oral and nasal cavities during the pronunciation of sounds.
Causes
The causes of rhinolalia can be congenital or acquired. Congenital causes of rhinolalia apply to children who have:
- clefts (non-fusion) of the soft and hard palate (“cleft lip”, “cleft palate” and others);
- short soft palate;
- muscle formation above the root of the tongue;
- paralysis or paresis (weakening) of the soft palate, manifested in the difficulty of raising and closing the palate with the back wall of the pharynx;
- flaccidity of articulatory muscles, which occurs in frequently ill children.
Clefts can be through, which involve not only the palate, but also the upper lip. They are one-sided and two-sided. Non-full nonunions are complete, which means they reach the incisor area without affecting the lips. Incomplete clefts are characterized by the fact that non-union occurs in a small area, for example, only in the area of the soft palate.
The acquired form of rhinolalia occurs with mechanical damage to the same areas and the face. In addition, the disease can develop due to tumor growths of the vagus and glossopharyngeal nerves.
For example, a functional open one appears in a person after surgery - removal of adenoids, various tumors and curvatures in the nasopharynx, with curvature of the nasal septum and the formation of polyps in the nasal cavity. In this case, the air practically does not enter the nose or enters there in insufficient quantities.
Closed rhinolalia can occur with adenoids, increased function of the muscles of the soft palate, which leads to isolation of the nasal and oral cavities from each other.
Acquired rhinolalia in a child can appear when a woman in the early stages of pregnancy suffered from viral diseases (influenza, rubella, mumps, dysentery, toxoplasmosis), had endocrine disorders, took certain medications, alcohol and smoked during pregnancy. Some researchers note the hereditary nature of such anomalies (my grandparents had clefts).
Symptoms of rhinolalia
The symptoms of the disease depend on its form.
With open rhinolalia, the child’s respiratory functions are impaired. Liquid food entering the cleft palate flows out through the nose, which significantly complicates the feeding process. In addition, the inhaled street air does not warm up to the required temperature, so children suffer from diseases such as otitis media, pneumonia, and bronchitis.
Due to open rhinolalia, children experience different types of developmental delays. For example, such a child begins to speak his first words late - usually after two years. Also, children have a pronounced nasal voice, making it difficult to pronounce sounds. Due to the fact that the root of the tongue is active during conversation, and not the tip, children pronounce most sounds deafly.
Closed rhinolalia is accompanied by rather unpleasant symptoms - mucus, formed in the upper respiratory tract, constantly flows down the back wall of the throat. Colds in this case rarely occur without snot, and the child has a chronic runny nose. Speech disturbances are also present. For example, a child pronounces the sound [b], but comes out [m].
According to many experts, speech defects lead to the development of asthenic syndrome and to some extent affect the child’s psyche; such children become withdrawn and have difficulty making contact.
- Such children are characterized by incorrect pronunciation of most vowels and consonants, their speech is slurred and inexpressive;
- Their voice is quiet, the timbre is dull and unnatural;
- If a child tries to carefully pronounce sounds, he begins to involuntarily grimace;
- At primary school age, such children always have problems with writing and reading.
Article:
Sometimes you can hear someone say about a baby: “They have some kind of autistic child!” Meaning that the baby is not sociable and avoids his peers.
In fact, autism is a disease that can only be diagnosed by a doctor. As well as other diseases associated with the mental and speech development of a child. Therefore, if in doubt, contact a psychologist, neurologist, or speech therapist. If the diagnosis is made by a specialist, then you can refer to our article, which briefly explains what this or the term means. Dyslalia is a defective pronunciation of certain sounds. At the same time, the child has a good vocabulary, he constructs phrases and sentences correctly. Simple training is important here. Dysarthria - with dysarthria, the pronunciation of all groups of sounds suffers. This is a pronunciation disorder caused by insufficient functioning of the nerves connecting the speech apparatus with the central nervous system (that is, insufficient innervation); Features of speech: “blurredness”, rhythm disturbance, inadequate intonation and tempo of speech. Here, the work of one speech therapist will not be enough. Observation by a neurologist is important. Rhinolalia is the so-called “nasal sound”. This is a violation of voice timbre caused by anatomical defects of the speech apparatus. Sometimes such pronunciation is provoked by adenoids and here a consultation with an otolaryngologist is needed.
Stuttering is difficulty in pronunciation. Violation of tempo, rhythm, fluency of speech caused by spasms of the muscles of the facial apparatus; occurs at the age of 2 - 2.5 years. Peculiarities: forced stops in speech, repetition of individual sounds and syllables, addition of extra sounds (“a”, “and”) before individual words. Prevention of stuttering: the speech of others should be unhurried, correct and distinct;
it is necessary to limit the child’s contacts with people who stutter;
do not allow scandals and conflicts in front of the child;
avoid mental and physical injuries (especially the head);
do not overload your child with information and impressions;
do not advance the child’s development and do not try to make him a child prodigy;
do not intimidate your child with scary fairy tales and all sorts of hedgehog grandmothers;
do not leave the child in a dark room as punishment, do not physically punish the child;
Alalia is a complete or partial absence of speech in children. It is important to consider age. You cannot give such a diagnosis to a 2-year-old child. Now, if from 3 to 5 years old a child still does not speak, then this is alalia. What causes the disease? Underdevelopment or damage to speech areas in the left hemisphere of the cerebral cortex, which occurs in the prenatal or early development of the child. Features: motor alalia - the child understands speech, but cannot reproduce it; sensory alalia - the child does not understand someone else’s speech; automatic repetition of other people's words is observed (instead of answering the question, the baby repeats the question itself). Observation by a number of doctors, including a speech therapist, will help overcome the disease.
Mutism is the cessation of speech development due to mental trauma. Features: general mutism - the child does not speak at all; selective mutism - with its silence the baby protests against any circumstances or people; Here, consultation with a psychiatrist and the help of a psychotherapist are important.
Childhood autism is a mental condition in which the child completely withdraws into his experiences and withdraws from the outside world; At the same time, basic everyday skills and speech are absent. Peculiarities:
- children are easily excitable and sometimes aggressive;
- often become fixated on something; such children may prefer a certain type of food not because of taste, but, say, because of appearance, and at the same time refuse other food offered; for example, a baby may not want to drink milk from a bag rather than from a carton;
- from the first months the baby does not strive to communicate with adults, does not cling to the mother;
- Such children are characterized by a feeling of danger; but their fears often have an unusual direction: a baby may be afraid, for example, of a desk, but not at all afraid of dogs or heights;
A neurologist, psychiatrist and psychotherapist will help the child at least partially adapt to his environment.
General speech underdevelopment (GSD) is a variety of complex speech disorders in which the formation of all components of the speech system is impaired, i.e. the sound side (phonetics) and the semantic side (vocabulary, grammar).
General underdevelopment of speech OHP is characterized by impaired pronunciation and discrimination of sounds, a small vocabulary, difficulty in word formation and inflection, and undeveloped coherent speech.
General underdevelopment of speech can be observed in complex forms of childhood speech pathology: alalia (always), as well as rhinolalia, dysarthria (sometimes).
Despite the different nature of the defects, children with OSD have typical manifestations that indicate systemic disorders of speech activity:
- later onset of speech (the first words appear by 3-4, and sometimes by 5 years);
- speech is not grammatically and phonetically structured enough;
- a child understands speech addressed to him, but cannot correctly voice his thoughts;
- the speech of children with ODD is difficult to understand;
There are three levels of speech development, which reflect the typical state of language components in OHP :
Level 1 - complete absence of speech or the presence of only its elements. Peculiarities:
- children's vocabulary consists of babbling words like “lyalya”, “bibi”;
- at the same time, one word can mean different concepts (“Lala” is both a doll and a girl);
- often the names of objects are used instead of the names of actions and vice versa: “tui” (chair) - sit, “pat” (sleep) - bed;
- such children do not know how to construct phrases; they say one-word sentences like “give”;
- many sounds are not pronounced;
- complex words are reduced to simple ones: “aba” (dog), “alet” (airplane);
2nd level. Peculiarities:
- a fairly large vocabulary; two-word and three-word phrases;
- the words used are heavily distorted and the connections between words in sentences have not yet been formalized; for example: “kadas ledit toy” (the pencil lies on the table);
- word agreement is broken; for example: “isa bezal” (the fox ran);
- in complex words, syllables are often rearranged or new ones are added; for example: “lisipede” (bicycle);
Level 3: characterized by a developed conversational phrase and the absence of gross violations in the development of various aspects of speech; however, there are disturbances in the formation of complex speech units. Peculiarities:
- incorrect use of endings and mismatch of words: “chairs” (chairs); “the slipper is lying” (the slipper is lying); "red sun" (red sun); “two buns” (two buns);
- simplification of complex prepositions: “from the table” (from behind the table);
- the vocabulary is quite large, but knowledge of nuances may be lacking (for example, the child may not know such parts of the body as the wrist, elbow, bridge of the nose);
- incorrect formation of diminutive forms: “stool” (chair); relative adjectives: “glassy” (glassy); possessive adjectives: “fox skin” (fox skin); and verbs with prefixes: “sew up a button” (sew on a button);
- the syllable structure of the word is reproduced correctly, with the exception of complex words; for example: “militsaner” (policeman);
- sounds are pronounced correctly, except for some complex sounds: “r”, “l”;
- sound analysis and synthesis are impaired (the child cannot distinguish the first and last sounds in a word, and is poor at selecting pictures for a given sound);
Possible causes of all the listed diseases and deviations from the norm:
- negative factors during pregnancy and childbirth;
- “pedagogical neglect” - a child, for various reasons, does not receive enough attention to himself; here we are talking not only about the lack of regular activities with the child, but first of all about communication with the child as a whole;
- perinatal encephalopathy (PEP) is one of the most common diagnoses; this concept unites brain lesions of different origins before, during or after childbirth; this diagnosis does not mean the child is inferior, but such a child needs a very qualified specialist;
- frequent illnesses, infections, injuries up to 3 years;
- hereditary factors;
- hearing loss;
- anatomical features of the maxillofacial apparatus;
- thumb sucking
Diagnosis of the disorder
As you can see, the symptoms of rhinolalia strongly overlap with many known diseases. Making a diagnosis is not as difficult as determining the type of disorder. To accurately diagnose the species, you need to consult a specialist. Examination of patients is carried out by various specialists in the field of medicine:
- maxillofacial surgeon;
- otolaryngologist;
- neurologist;
- orthodontist;
- speech therapist;
- orthopedist;
- psychologist.
Research methods depend on the form of rhinolalia. When identifying different types of rhinolalia, special attention is paid to x-rays of the nasopharynx.
The sooner a child is diagnosed with rhinolalia, the sooner treatment can begin. Correcting a neglected form is much more difficult.
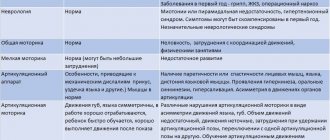
During an examination by a speech therapist, a specialist assesses the structure of the articulatory apparatus, the pronunciation of sounds, the understanding and use of words, and the presence of agrammatisms in speech.
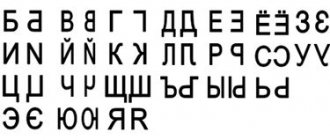
Rhinolalia (its open form) is diagnosed based on Gutzman's research, when when pronouncing the vowel sounds [a] and [i], the child alternately begins to close or open the nasal passages. In school-age children, the specialist also examines the processes of writing and reading, which clearly indicate the presence and level of the problem.
Correction of rhinolalia at a speech therapy center in Moscow
Corrective work with children with rhinolalia should begin when a problem is detected in order to achieve positive results by adolescence. Depending on the form, speech therapy work can be the main or complementary work of other specialists.
The role of a speech therapist for rhinolalia is to consolidate sound pronunciation skills. Massage is used, the development of velopharyngeal closure, the development of exhalation and sound pronunciation, the elimination of nasality, the development of vocabulary and work on lexical literacy.
- Correction for functional rhinolalia. A positive effect can be achieved through sessions with a speech therapist. They include massage, breathing exercises, work on developing the correct pronunciation of sounds and auditory attention.
- Correction for organic form. The effectiveness depends on the surgical intervention, the timeliness of the operation and the completeness of the speech therapist’s work with the child.
Correction methods
Treatment of rhinolalia includes a whole range of measures aimed at maximizing the elimination of speech defects.
If a child is diagnosed with congenital rhinolalia, then correction of the disorder begins with the elimination of defects of anatomical origin. From birth, such children begin to be fed using a tube, which is selected taking into account the characteristics of the cleft.
A special prosthesis, an obturator, is also made to close the nonunion. This prosthesis facilitates the processes of eating, breathing and speaking.
Late use of an obturator is less effective, since the child begins to develop incorrect tongue position with age. The obturator changes as the child grows and is used until the moment of surgical intervention, which, unfortunately, cannot be done without.
Maxillofacial disorders are subject to surgical intervention. Nasality with open rhinolalia is treated both before and after surgery.
As a rule, cleft lip surgery is performed at 2–3 months of a child’s life. Operations on the palate are carried out after two years, if the child has lost all his teeth. In weakened children, surgery is postponed to a later date or carried out in several stages.
Surgeries allow you to restore the integrity of the speech apparatus and the proper functioning of the palate.
Articulation exercises
To correct articulation disorders caused by rhinolalia, special exercises are needed:
- “Snake or spade” - you need to learn to stick out your tongue with a pointed tip, and then widely flattened. The next stage is to alternate between “snake” and “shovel”.
- “Bend the back” - the tip of the tongue rests on the lower gums, and the back of the tongue curves up and down.
- “Inflate and deflate” - the cheeks need to be inflated and deflated, pulling them between the teeth. As an option, learn to inflate not both cheeks at once, but alternately. An adult can help deflate the puffy cheek by lightly touching it with a finger.
- “Rinse your teeth” - imitate rinsing your teeth without water (the air should press on your lips).
- “Elephant exercise” - the child must learn to hold his lips closed and extended forward with his “proboscis”, and then move it left and right and even rotate it.