Apraxia is a partial or complete impairment of the mobility of individual parts of the body or muscle groups while maintaining the conductivity of nerve endings and a normal level of intellectual development. This pathology can develop in children of all age groups due to organic damage to brain tissue or the conductive channels of the corpus callosum.
Apraxia can manifest as various dysfunctional disorders of all parts of the body. In speech therapy, this disease implies a violation of the normal development of the speech apparatus, when the child is unable to pronounce sounds, words or construct correct sentences.
Apraxia of this type most often occurs in children of the younger age group during the period of their active development. A distinctive feature of apraxia is that the child maintains stable mental development, he perceives and assimilates information well, and the functions of the peripheral nervous system are preserved in terms of the conduction of neural impulses in the brain.
At the same moment, due to focal lesions of the central nervous system, a disturbance in the motor activity of that part of the body for which a certain part of the brain hemisphere is responsible occurs.
The severity of apraxia depends on the severity of damage to the central nervous system. Disturbances in the development of the speech apparatus in children of the younger age group are caused by local damage to the frontal lobes of the brain.
Kinds
Apraxia is a neurological disease that comes in many varieties. Each type of this pathology is distinguished by its individual symptoms, as well as the localization of focal damage to brain tissue.
Apraxia in speech therapy. Types of disease.
In this case, the development of the disease may be due to the negative influence of various factors.
Frontal
Frontal apraxia is characterized by damage to the prefrontal areas of the cerebral cortex in the frontal lobe. The disease is characterized by severe impairment of complex and sequential movements. Moreover, this type of apraxia can be limited or total in nature with dysfunction of individual groups of muscle fibers, or with absolute immobility of the limbs. Frontal apraxia can develop as a consequence of a stroke or severe trauma to the skull.
Motor
The motor type of apraxia is characterized by the fact that the child is able to independently formulate an action plan for performing certain tasks, but is not able to fully realize the functions of individual elements of the musculoskeletal system. In this case, the patient requires help from strangers (for example, lifting a toy or moving any environmental object).
Premotor
Premotor apraxia occurs in children who have signs of damage to the premotor areas of the cerebral cortex. A more detailed examination of the patient reveals that the child has symptoms of inertia and lack of automation of movements. Children with premotor apraxia can perform elementary motor acts, but lack the ability to transform them into more complex actions.
Cortical
This type of apraxia develops in case of damage to the tissues of the dominant hemisphere of the brain.
In this case, the pathological condition of the central nervous system can be manifested by disturbances in the motor activity of the limbs or muscle groups on only one side of the body.
Bilateral
Bilateral apraxia is the result of severe bilateral damage to the cerebral hemispheres. In this case, the main focus of pathology is localized in the parietal region of the central nervous system. The disease is characterized by multiple dysfunctions of the musculoskeletal system.
Akinetic
Akinetic apraxia is a separate type of this neurological disorder in which the child’s psychomotor activity is affected. The main manifestation of the pathology is the complete or partial absence of stimulation of the central nervous system to active movements, to perform certain actions that are necessary to achieve set goals. This type of disease is detected in the early period of child development.
Amnestic
Amnestic apraxia is characterized by complete or partial loss of the ability to perform independent voluntary actions. At the same time, the child actively imitates the behavior of adults and other children in his immediate environment.
This type of pathology negatively affects not only the physical development of the patient, but also leads to impairment of the psychomotor and cognitive functions of the brain.
Ideatorial
Ideation apraxia is different in that, due to focal lesions of certain areas of the central nervous system, the child is not able to independently outline a clear plan of action to complete the assigned tasks. The symptoms of this pathology appear especially clearly when children with a similar diagnosis try to implement complex motor acts.
Ideokinetic
Ideokinetic apraxia is a neurological disorder in which a child is able to perform random movements of individual parts of the body or muscle groups, but is unable to carry out simple actions that develop into a more complex motor act. In terms of symptoms, this type of disease resembles cerebral palsy with signs of periodic remission.
Kinesthetic
Kinesthetic apraxia develops in children who have damage to the postcentral part of the central nervous system with the spread of pathology to the dominant hemisphere of the brain. This type of disease leads to disturbances associated with the performance of voluntary movements. The child cannot independently decide what actions he needs to perform in a particular situation.
Constructive
Constructive apraxia affects the cognitive functions of the brain. A child with this type of neurological disorder is not able to independently assemble a separate object from its component parts. For example, collect a multi-colored cube, or an elementary picture consisting of several puzzles.
Apraxia
This type of disease develops in children who have focal lesions of the cerebral cortex in the parieto-occipital region. Most often, the right hemisphere is in the zone of a progressive pathological process. Apraxia of dressing is characterized by the fact that the child completely or partially lacks the ability to dress independently.
Oral apraxia
Oral apraxia is a series of disorders of the motor activity of the facial muscles, motility of the lips and tongue tissues, which ultimately leads to the absence or improper development of the speech apparatus. In speech therapy, this type of pathology is considered a serious disease that is difficult to treat.
The severity of oral apraxia depends on the extent of damage to the centers of the brain.
Spatial
This type of neurological disorder is distinguished by the fact that as the child grows up, he does not develop the ability to navigate in the surrounding space. This pathology may be accompanied by attacks of dizziness and a lack of understanding of simple things that are necessary for independent movement. For example, a child is already quite old and cannot understand where the right or left side is.
Apraxia of walking
Apraxia of gait is a neurological disorder in which the child has preserved the functions of all elements of the musculoskeletal system, there are no symptoms of vestibular disorders, but there are clear signs of walking impairment. A similar pathology occurs in children with local lesions of the frontal lobe of the brain.
Principles of therapy
Corrective work for dyspraxia is based on the integrated use of therapeutic measures.
Drug treatment
The use of medications is aimed at eliminating the cause of the pathology and reducing the severity of symptoms. For secondary forms of dyspraxia, appropriate treatment is selected - for neuroinfection, antibacterial or antiviral agents are prescribed; for brain tumors - chemotherapy and radiation therapy.
The following are used as drugs that affect the nervous system:
- nootropics (Phenotropil, Piracetam, etc.) - improve metabolic processes in neurons and increase their resistance to negative influences (with a course of drugs, cognitive skills improve, including motor and speech);
- Actovegin and Cerebrolysin - improve blood flow in the vessels of the brain, leading to an increase in the amount of nutrients and oxygen delivered;
- Taxifolin, Tocopherol and other antioxidants protect nerve cells from adverse factors.
Non-drug methods
In speech therapy and neurology, non-drug approaches are actively used to eliminate the symptoms of dyspraxia. A positive effect is observed from therapeutic massage, physical therapy and swimming. These effects normalize muscle tone and help improve fine motor skills.
If available, electrical muscle stimulation, transcranial stimulation of the cerebral cortex, passive vestibular training and other kinesiotherapy techniques are performed in a medical institution. The procedures teach the patient the correct motor pattern.
Exercises for the development of speech and motor skills
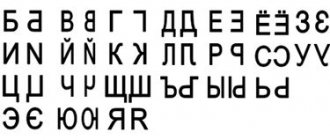
Speech therapy exercises are aimed at two main aspects of speech:
- improving the correct pronunciation of phonemes and their combinations;
- training the muscles involved in the articulation process.
The following tasks are recommended:
- exercises to strengthen the muscles of the tongue: you need to roll it up into a tube, pull it forward, fold it into a “cup”, etc.;
- task “centipede race” - children run a race with their hands on the table, competing with each other;
- collecting paper airplanes and flying distance competitions;
- puzzle game;
- repeating a certain facial expression after a specialist with an explanation of the emotions that are characteristic of it;
- “walking with hats” - the child puts a small load on his head (a book, a pyramid stand) and competes with other children in terms of walking distance.
Experts identify several dozen exercises for developing correct phonetics and motor skills. They are carried out together with a speech therapist or independently at home after training. The duration of corrective measures depends on the severity of symptoms. For minor violations, the duration of classes is 1-3 months. If significant speech and motor defects are observed, treatment is required for 6-12 months under the supervision of a specialist.
Symptoms and signs
Apraxia in speech therapy is a dysfunction of certain brain centers that are responsible for the motility of the facial muscles, synchronous mobility of the lips and tongue tissues. The first signs of pathology appear in the early stages of a child’s development and also depend on his age.
In children under 3 years of age
In a child of this age group, the main signs of apraxia are the following deviations in the development of the speech apparatus:
- in infancy, children with this pathology do not babble, and also do not make any other attempts to verbally express their emotions;
- the first simple words appear too late, or are completely absent, despite the fact that, due to his age, the child should already be able to pronounce them (for example, mom, dad, baba);
- when trying to speak, a child with oral apraxia is able to produce only a few consonant or vowel sounds that are unintelligible and do not resemble words;
- when pronouncing sounds, the child makes too long pauses;
- in the presence of mild oral apraxia, the child is able to reproduce individual simple words, but at the same time replaces sounds that are difficult to pronounce with easier ones.
Oral apraxia in children of this age group may be accompanied by an unauthorized change in the structure of the word. For example, when a child pronounces the names of objects in a way that is more convenient for him to pronounce the letters of which they are composed. The presence of such symptoms should be the first alarming signal for the child’s parents and kindergarten teachers. In this case, immediate involvement of a speech therapist is required.
In children over 3 years old
Apraxia in speech therapy is a dysfunction of the brain centers that are responsible for the full functioning of the speech apparatus.
In children over 3 years of age, the symptoms of this pathology manifest themselves as follows:
- the child makes immediate mistakes in the process of reproducing sounds, which are not signs of age-related immaturity;
- children with a similar disease understand the language of the people around them, understand the meaning of the words that are spoken to them, but at the same time cannot repeat what was said;
- there are pronounced signs of imitation in the reproduction of heard words, during which this speech is clearer than words spoken after making an independent conclusion;
- hypersensitivity or too low sensitivity of tissues located in the corners of the mouth;
- while attempting to say a word or reproduce a sound, the child gropes certain parts of the face and touches the surface of the lips, which indicates complete or partial dysfunction of the motor skills of these parts of the body;
- poor assimilation of information that comes from loved ones or teachers of educational institutions;
- impairment of fine motor skills of the upper limbs;
- with partial oral apraxia, the child manages to pronounce simple and short words, but at the same time he faces significant difficulties when pronouncing complex word combinations (the ability to construct sentences is practically absent).
The above symptoms can be aggravated at a time of excitement or the presence of a new person in the child’s immediate environment. Children over 3 years of age who suffer from mild oral apraxia may have irregular, choppy, or severely slurred speech. Quite often, children with signs of pathologies of the speech apparatus have other developmental disorders. For example, problems with learning to read, write, dysfunction of muscle groups of the musculoskeletal system.
Study
Many researchers are studying the characteristics of apraxia of speech and the most effective treatment methods. Below are a few recent discoveries:
Sound production processing:
Articulatory-kinematic treatments have strong evidence for their use in the treatment of acquired apraxia of speech. These treatments use relief of movement, positioning, timing, and articulation to improve speech. Sound production processing (SPT) is an articulatory-kinematic processing that has received more research than many other methods. It combines modeling, repetition, minimal paired contrast, integral stimulation, articulatory cueing, and verbal feedback. It was developed to improve the articulation of target sounds in the mid-1990s. SPT shows consistent improvements in trained sounds across trained and untrained words. The best results are achieved when using eight to ten instances of the target sound, which facilitates generalization to untrained samples of trained sounds. Additionally, maintenance effects are strongest 1-2 months after treatment, when sounds achieve high fidelity during treatment. Therefore, treatment termination should not be determined by effectiveness criteria or the number of sessions the client has completed to have the greatest long-term effect. Although there are many parts of SPT that require further study, it can be expected to improve the production of target sounds for speakers with apraxia of speech.[24]
Repeated practice and routines to control speed/rhythm:
Julie Wambau's research focuses on clinically applicable treatments for acquired apraxia of speech. She recently published a paper examining the effects of repeated practice and speed/rhythm control on sound production accuracy. Wamba and colleagues studied the effects of this treatment in 10 people with acquired apraxia of speech. The results show that repeated hands-on treatment results in significant improvements in articulation for the majority of clients. Additionally, speed/rhythm control helped some clients but not others. Thus, incorporating repeated treatment practice into therapy is likely to help people with AOS.[25]
Nuffield Dyspraxia-3 Program (NDP-3) and Rapid Syllable Change Treatment (Rest):
A 2021 Cochrane review found that, when used intensively, both NDP-3 and ReST can improve word accuracy in children aged 4 to 12 years with CAS.[26]
Causes
Apraxia in speech therapy is a neurological disorder that must be detected as early as possible. The main reason for the development of this pathology is the presence of focal damage to areas of the central nervous system responsible for the mobility of the muscles of the face, lips and tongue.
The development of such a disease can provoke the negative impact of the following factors:
- damage to the fetal brain by infectious microorganisms that were able to overcome the placental and blood-brain barrier;
- damage to the central nervous system by chemical or biological substances that have pronounced toxic properties;
- birth trauma of the skull, or brain damage resulting from a fall from a great height or blows;
- pathological influence of drugs and alcoholic beverages, if the child’s mother had harmful addictions throughout the entire period of intrauterine development of the fetus;
- abnormalities of intrauterine development;
- genetic predisposition, if similar pathologies of the cerebral cortex were previously encountered in blood relatives of the child’s parents.
The causes of oral apraxia or another type of this disease can be determined by a neurologist at the stage of preliminary examination of the child in order to establish the nature of the origin of dysfunctions of the speech apparatus.
Gesture prompts
Another approach is to use visual gesture cues. The parent or therapist touches their mouth when they make a certain sound. For example, we can bring our index finger to our lips and move it away when we say the sound "p". The prompt draws the child's attention to how the lips form a certain sound.
We will use more than one clue when we say a whole word to show the difference between the sounds in a word. The combination of visual and verbal cues helps the child focus, understand and pronounce the word better.
This type of prompting can be especially helpful for children with autism, who often tend to be visual learners. However, this method requires that the child can pay attention to the cues and imitate them.
Diagnostics
Diagnosis of apraxia is carried out with the participation of an audiologist and speech therapist. A specialist of the first profile assesses the child’s hearing level in order to exclude pathologies of the inner ear, the presence of which affects the quality of development of the speech apparatus. After this, a certified speech therapist who has practical experience working with children suffering from apraxia begins to examine the patient.
The table below describes the main types of examination techniques that are used to make a final diagnosis:
| Type of diagnosis of oral apraxia | Principle of the survey |
| Oral-motor assessment | An oral-motor assessment involves diagnosing signs of low tone of muscle tissue responsible for the mobility of certain areas of the face, lips, lower jaw or root of the tongue. During the diagnosis, the speech therapist asks the child to show how he moves his tongue from the right to the left, and whether he can touch its tip to the surface of the palate. Assessment of the level of coordination of movements of all elements of the speech apparatus is carried out by repeating complex phrases or playing a number of sounds. For example, quick pronunciation of tongue twisters, or simple words in the form of “pah-tuh-kah”. At the moment when the child reproduces test words and sounds, the speech therapist monitors the mobility of the patient’s lips, tongue and facial muscles. |
| Melody of speech | Assessment of speech melody is one of the stages of complex diagnosis of children with signs of this disease. The specialist listens carefully to the words and sounds that the child reproduces, paying special attention to the correct composition of syllables. The main purpose of assessing the melody of speech is to determine the patient’s ability to form sentences of various types (interrogative, narrative). |
| Speech sounds | This method of diagnostic examination, which is also carried out by a speech therapist, involves assessing the ability to pronounce consonants and vowels. The specialist asks the child to reproduce individual words that contain the largest number of sound combinations. Based on the results of communication, an appropriate conclusion is drawn up about the presence or absence of oral apraxia. If this diagnosis is confirmed, the severity of the neurological disorder is assessed. |
The average cost of a comprehensive examination by a speech therapist is 1,100 rubles. The duration of diagnosing a child for the presence of apraxia varies from 45 minutes. up to 1 hour
Recommendations
- West, Caroline; Hesketh, Anne; Vail, Andy; Bowen, Audrey; West, Carolyn (2005). “Interventions for apraxia of speech after stroke.” Cochrane Database Syst Rev
(4): CD004298. Doi:10.1002/14651858.CD004298.pub2. PMID 16235357. - ^ a b c d f f
“Apraxia of speech.”
National Institute on Deafness and Other Communication Disorders
. National Institutes of Health. Retrieved April 12, 2012. - Morgan AT, Vogel AP (March 2009). "A Cochrane review of the treatment of apraxia of speech in children." Eur J Phys Rehabil Med
.
45
(1): 103–10. PMID 19156019. - Varga-Khadem F, Gadian DG, Kopp A, Mishkin M (February 2005). "FOXP2 and the Neuroanatomy of Speech and Language" (PDF). Nat.
Rev. Neurosci .
6
(2): 131–8. Doi:10.1038 / No. 1605. PMID 15685218. S2CID 2504002. - Maassen, B. (November 2002). "Issues contrasting adult acquired apraxia of speech and developmental apraxia." Semin Speech Language
.
23
(4): 257–66. doi:10.1055/s-2002-35804. PMID 12461725. - ^ a b c d e g
Ogar J., Slama H., Dronkers N., Amici S., Gorno-Tempini M.L.
(December 2005). "Apraxia of speech: a review." Neurocase
.
11
(6): 427–32. Doi:10.1080/13554790500263529. PMID 16393756. S2CID 8650885. - ^ a b c d e
Knollman-Porter, K. (2008).
"Acquired apraxia of speech: a review." Upper Stroke Rehabil
.
15
(5): 484–93. Doi:10.1310/tsr1505-484. PMID 19008207. S2CID 1664688. - ^ a b c
Rosenbeck, John S.;
Wertz, Robert T.; LaPointe, Leonard L. (1984). Apraxia of speech in adults: a disorder and treatment
. New York: Grune & Stratton. ISBN 978-0-8089-1612-3. OCLC 13284954. - van der Merwe, Anita (June–August 2007). “Self-Correction for Apraxia of Speech: Effect of Treatment” (PDF). Aphasiology
.
21
(6–8): 658–669. Doi:10.1080/02687030701192174. - Boutsen, F. R.; Christman, S. S. (November 2002). "Prosody in apraxia of speech." Seminars in Speech and Language
.
23
(4): 245–56. doi:10.1055/s-2002-35799. PMID 12461724. - ^ a b
“Apraxia of speech.” American Speech-Language-Hearing Association. 2013. - Josephs CA, Duffy Jr (December 2008). "Apraxia of speech and shallow aphasia: a new clinical marker of corticobasal degeneration and progressive supranuclear palsy." Current Opinion in Neuroscience
.
21
(6): 688–92. Doi:10.1097/WCO.0b013e3283168ddd. PMID 18989114. S2CID 34877712. - ^ a b
Josephs K.A., Duffy J.R., Strand E.A.
and others (May 2012). "Characteristics of a neurodegenerative syndrome: primary progressive apraxia of speech." Brain
.
135
(Pt 5): 1522–36. doi:10.1093/brain/aws032. PMC 3338923. PMID 22382356. - Ricci M., Magarelli M., Todino V., Bianchini A., Calandriello E., Tramutoli R. (2008). "Progressive apraxia of speech as an isolated disorder of speech articulation and prosody: a case report." Neurocase
.
14
(2): 162–8. Doi:10.1080/13554790802060839. PMID 18569741. S2CID 31167113. - Krut, K. (November 2002). "Diagnostics of AOS: definition and criteria." Seminars in Speech and Language
.
23
(4): 267–80. doi:10.1055/s-2002-35800. PMID 12461726. - Ziegler, W., Eichert, I., & Steiger, A. (2012). American Speech-Language-Hearing Association Supplement: Apraxia of Speech: Concepts and Controversies. Journal of Speech, Language and Hearing Research, 55, 1485–1501.
- Janet Choi J, Thompson SK (May 2010). "Binding in agrammatic aphasia: Processing to comprehension." Aphasiology
.
24
(5):551–579. Doi:10.1080/02687030802634025. PMC 2882310. PMID 20535243. - Robin DA, Jacks A, Hageman S, Clark HM, Woodworth G (August 2008). "Visuomotor tracking abilities of speakers with apraxia of speech or conduction aphasia." Brain Lang
.
106
(2):98–106. doi:10.1016/j.bandl.2008.05.002. PMC 2579757. PMID 18558428. - Carlson, Neil R. (2010). Psychology: The Science of Behavior
. Canada: Pearson Education. ISBN 978-0205702862. - "Dysarthria." American Speech-Language-Hearing Association.
- Mauszycki, Shannon C.; Wambaugh, Julie (2011). "Acquired apraxia of speech: a review of treatment." American Speech-Language-Hearing Association (ASHA). Archived from the original on August 13, 2013. Retrieved October 20, 2013.
- "Archival copy." Archived from the original on 02/22/2014. Retrieved 2014-02-13.CS1 maint: zipped copy as title (link)
- Howard, Sarah; Varley, Rosemary (1995). "III: EPG in Therapy Use of Electropalatography for the Treatment of Severe Acquired Apraxia of Speech." International Journal of Language and Communication Disorders
.
30
(2): 246–255. Doi:10.3109/13682829509082535. PMID 7492855. - Wambaugh, J. (2010). “Sound Treatment for Acquired Apraxia of Speech” (PDF). Perspectives on neurophysiology and neurogenic speech and language disorders
.
20
(3): 67–72. Doi:10.1044/nnsld20.3.67. Archived from the original (PDF) on 2013-12-03. - Wambaugh J.L., Nessler S., Cameron R., Maushitsky S.K. (May 2012). "Acquired apraxia of speech: Effects of repeated practice and rate/rhythm control procedures on sound production accuracy." Am J Speech Lang Pathol
.
21
(2):S5–27. Doi:10.1044/1058-0360(2011/11-0102). PMID 22230177. - Morgan, Angela T.; Murray, Elizabeth; Liégeois, Frederic J. (May 30, 2021). "Interventions for childhood apraxia of speech." Cochrane Database of Systematic Reviews
.
5
: CD006278. Doi:10.1002/14651858.CD006278.pub3. ISSN 1469-493X. PMC 6494637. PMID 29845607.
Treatment methods
Apraxia in speech therapy is a complete or partial dysfunction of the speech apparatus, which excludes the full development of the child. The main and only treatment for oral apraxia is regular sessions with a certified speech therapist. To achieve a positive effect in reducing the severity of pathological symptoms, as well as improving speech, the child should attend 3 to 5 therapeutic sessions per week.
Classes with a speech therapist are conducted on an individual basis, depending on the severity of apraxia or the clinical manifestations of this disorder.
For example, if a child cannot pronounce a certain set of sounds, then the specialist draws up a lesson plan so as to emphasize the reproduction of words where there is a defective sound. In addition, regular sessions with a speech therapist can prevent atrophy of the muscles responsible for facial expressions, mobility of the lips, tongue or lower jaw.
The duration of therapy depends on the dynamics of restoration of normal functions of the child’s speech apparatus. The average cost of 1 lesson with a speech therapist is 700 rubles.
Identifying apraxia of speech
So what might indicate that your child has apraxia of speech? Children with apraxia have difficulty coordinating the movements of the tongue, lips, mouth, and jaw to produce distinct and consistent speech sounds. So every time such a child says a word, it may sound different. Because of this inconsistency in pronunciation, even parents who know all the features of a child’s speech may find it difficult to understand him.
Experts cannot always determine why a child has difficulty speaking. A developmental disorder like autism makes this even more difficult because it involves communication problems. So if you have any such concerns, we recommend that you seek evaluation from a professional speech therapist. It is speech therapists who must be trained to differentiate between different speech disorders, which can be very similar. They can also develop a customized plan to overcome the problem.
Possible consequences and complications
The lack of treatment aimed at restoring and improving the quality of a child’s speech threatens the development of the following complications and negative consequences:
- violation of the child’s socialization;
- progression of dysfunction of the facial muscles, which is responsible for the mobility of the lower jaw, lips and tongue (this complication will only aggravate the existing signs of oral apraxia);
- the need to receive individual education due to the lack of ability to reproduce words and correctly construct sentences;
- retardation in physical and mental development;
- lack of communication skills with peers and other people around them;
- the emergence of a tendency to aggression, the emergence of outbursts of rage and signs of an unstable psycho-emotional state due to limited abilities to express thoughts;
- the development of complexes and self-doubt that appear in a child due to incorrect reproduction of words and sounds, as well as ridicule from other children;
- preservation of speech apparatus defects, which remain with children at all stages of their growing up, significantly reducing their quality of life.
Apraxia is a severe neurological disorder that develops due to focal lesions in individual areas of the central nervous system. In speech therapy, this disease is characterized by oral apraxia, the symptoms of which are manifested by impaired mobility of the facial muscle tissues responsible for the synchronous interaction of the lips, lower jaw and tongue.
The main symptom of this disease is that the child completely or partially lacks the ability to reproduce most sounds and words. An audiologist and speech therapist are involved in diagnosing pathology.
Gradation according to A. R. Luria
Four types of apraxia according to Luria:
- Regulatory. The prefrontal areas of the brain are affected. The patient has a violation of speech regulation, control over the flow of movements is lost. He cannot cope with motor tasks, repeats actions, and finds it difficult to learn a new program. Some skills are lost, some patterns remain. The result of the activity does not coincide with the plan.
- Spatial. The parieto-occipital regions are affected (typical of the left side). Spatial-visual contacts of movements are impaired, switching from operation to operation is difficult. Spatial movements (washing, cooking, dressing) are not easy to perform, which makes everyday life difficult. It is difficult for the patient to relate his body to the world around him.
- Kinetic. The lower part of the premotor area is affected. Smooth switching from movement to movement is disrupted. The patient literally “gets stuck” as soon as he begins to move. Writing skills are also impaired.
- Kinesthetic. The lower parietal zone is affected, most of all the left hemisphere. Impaired afferentation, it is impossible to give the body the desired position. The patient does not feel his fingers or hands, hence the impairment of writing skills and object actions.
Building a Basic Dictionary
With this and other approaches, it is very important to always start with the basic vocabulary. This is the name of 10-20 words that parents and specialists choose
The main dictionary should include those words that are most often used in everyday speech (for example, “mom” and “dad”), have a special meaning for the child (for example, “train”, if the child really loves trains), and indicate the most common actions (for example, “eat”, “go”, etc.) and which are easiest to imitate (depending on the child’s skills).
Together with a specialist, the child will practice pronouncing these words in structured lessons. At home, you will practice saying these words in natural situations when the child encounters these people, objects or actions throughout the day.
As with any new skill, constant repetition and practice is the best way to improve results and help your child become more independent. At first, your child may need help pronouncing the word. Then gradually she learns to say it on her own without your prompting. After this we can enter a new word to form a phrase and so on.
Typically, therapy for apraxia is a combination of all of these approaches.
Prevention
Preventive measures that effectively help prevent this problem have also not been developed. Despite this, there are a number of recommendations that significantly reduce the risk of the occurrence and development of movement disorders:
- giving up bad habits and alcohol;
- make regular walks in the fresh air and exercise;
- regulate your diet;
- eat a balanced diet, consume only healthy foods and in quantities necessary for the body;
- visit the hospital regularly and undergo a full examination;
- Monitor your blood pressure and if surges are observed, it is better to consult a doctor about this problem.
Apraxia is a rather complex and serious disease, as a result of which a person loses the motor function of certain organs or parts of the body, and it is difficult for him to carry out even the most basic manipulations with objects.
People suffering from this disease are dependent on society, in particular on family and friends, since they are simply unable to perform certain operations. Be healthy!