Sample psychological, pedagogical and speech therapy characteristics for a child with motor alalia
Tweet
Ponomareva Elena Vitalievna
teacher-speech therapist MBDOU D/s No. 31
Kamyshin
General information about the child: Lesha K., born ....., attends MBDOU D/s No...., attends kindergarten for the third year.
Study of anamnesis: Child from 4th pregnancy. During pregnancy, the mother was in confinement, complaining of toxicosis. Premature birth is rapid. Asphyxia, hypoxia, ischemia. Features of early development: holds head from 3 months, sits from 7 months, walks from 1 year 2 months. Mom could not remember the features of early speech development. First words at 4 years old (ma, pa, ba). The parents do not have hereditary neuropsychiatric diseases. Diseases of the first year of life: frequent acute respiratory viral infections. Hearing and vision are normal.
Conditions of family upbringing: Raised in a complete family, but dad works in another city. The mother works in a factory and pays little attention to the child. There is an older brother (15 years old) with speech development corresponding to the age norm. The family has a grandmother who spends more time with the child than other family members. She sincerely loves the child, but due to illiteracy, she cannot provide Lesha with the necessary developmental speech environment. All family members are Russian-speaking.
Self-care skills at a high level: he washes his hands and wipes himself with a towel. Dresses and undresses without help. He folds his clothes. Eats independently. Holds cutlery correctly.
Game activity: In the game, as a rule, occupies a subordinate position. Constantly imitates children. Tries to attract children's attention, sometimes takes away their toys. Sometimes he asks: “Give me a bib.” Often plays alone.
Motor-motor development: Motor activity is at an average level. Motor clumsiness, gets tired quickly. Fine motor skills of the hands are underdeveloped: Lesha performs shading with violations of the contour of the drawing. He ties the strings on his hat on his own, but with difficulty, and his movements are slow and awkward.
Prerequisites for educational activities: Performs tasks according to step-by-step instructions from an adult and together with an adult. Self-control skills are poorly developed.
Cognitive processes:
-attention: sometimes has difficulty concentrating and switching attention to tasks proposed by adults. Shows interest in the task being performed, but copes with tasks and exercises only with an individual approach from an adult. The rate of work capacity is low, which is associated with absent-minded attention and very rapid fatigue.
-perception: knows and shows correctly the primary colors. Correctly correlates geometric shapes with the sample. Folds cut pictures from 2, 3, 4 parts (including diagonally). Correlates objects relative to size through trial and error and with the help of an adult.
- memory: visual memory predominates. The memory capacity is small. Memorization is short-term, even if a memorization setting has been given.
-thinking: can perform basic logical operations, sometimes accompanied by an adult. It is difficult to classify objects according to the main characteristic; it does not build cause-and-effect relationships. Most often, Lesha manages to cope with tasks that do not require reasoning or do not require answers.
- imagination: reproductive.
Personality characteristics:
— motivational-need sphere: Often the instructions for the task are not understood the first time. A child often needs support and praise from an adult. All tempo characteristics are slightly reduced.
— emotional-volitional development: the prevailing mood is neutral. There is no clear expression of any emotions. He is not capricious. A smile appears on the face rarely, fleetingly. Children do not offend him, but if this happens by chance, then Lesha simply withdraws from the game.
- communicative activity: Lesha is “accepted” in the peer group. Not proactive. Accepts the terms of a group game proposed by an adult. He is contactable with children and well-known adults, but with unfamiliar adults he is silent and withdraws into himself.
- individual characteristics, character traits: the child is balanced, friendly. He is diligent, but his activities are most often ineffective, as he gets tired very quickly. The material is absorbed in small portions and slowly. All tempo characteristics are reduced.
Features of speech development:
-vocabulary: The passive vocabulary is much wider than the active one. A good understanding of the speech addressed to him not only at the everyday level, but also in specially organized classes. Words available in the active dictionary: one-syllable (give, where, on), two-syllable (mom, aunt, bye, autumn). Very rarely uses simple, uncommon sentences (Auntie, bye. Where is uncle? Give me bibi.) Speech is of an everyday nature. The verb dictionary is characterized by insufficiently formed ideas about the actions being performed and their differentiation. A high-quality dictionary is characterized by the absence of adjectives that describe the color, shape, and size of objects.
-grammatical structure of speech: Uses nouns and verbs in the infinitive form. There is no agreement between words in the sentence. Does not form plural nouns. I.p.. Word formation is not available. Understands, but does not use prepositions in speech: on, in and many others.
— sound pronunciation: violation of sound pronunciation is polymorphic in nature.
- syllable structure: grossly violated. Speech is unclear
- prosodic side of speech: the voice is quiet, unemotional. Speech is slurred.
-structure and mobility of the articulatory apparatus, presence of hesitations: performs articulatory exercises with errors, long search for a pose, distortion of the articulatory posture.
- phonemic perception, analysis and synthesis: phonemic processes, as well as the skills of sound analysis and synthesis are not formed.
— formation of coherent speech: not formed.
Speech therapy conclusion:
OHP level 1. Motor alalia.
Long-term plan for correctional work with a child:
Stage I. Nurturing speech activity, forming a passive and active vocabulary accessible to understanding and perception. Dialogue, a short story, a simple unexpanded and a common sentence are used. Stage II. Formation of phrasal speech: - distribute the proposal on specific issues, on the didactic elements of the phrase, presented visually; - formulate sentences intonationally and grammatically; - work to complicate the structure of the phrase; — complication of the dictionary due to abstract words; - dialogue, descriptive stories (description of one object, group of similar objects, compare descriptions of different objects). Stage III. Formation of coherent speech as a particularly difficult communicative activity. - the method of breaking it down into parts that are accessible for perception and repetition is used; — work on the coherence and integrity of the text; - creative storytelling in likeness; — texts and pictures with more complex content; — when working on a text with a hidden meaning, speech and semantic activity is trained. Speech exercises: - perception of a finished sample, - analytical types of work (highlight a specific word), - construction of words (insert a specific one! to the word), = the child learns to reason, generalize, draw conclusions. A) practical, b) visual and c) verbal methods are used: a) games, exercises, modeling (game methods + demonstration, question, instruction, explanation). b) drawings, observation, c) story, conversation, explanation, pedagogical assessment.
Share on social media networks
I like
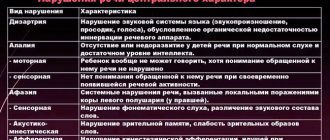
Alalia classification
Each area of clinical medicine has its own narrow classification of alalia, which is based on the causes of occurrence, existing pathologies of psychomotor development and the degree of speech underdevelopment.
Modern speech therapy suggests taking as a basis the classification of alalia by V.A. Kovshikov:
- Motor (expressive).
- Sensory (impressive).
- Mixed (sensorimotor).
Expressive alalia
In most cases, motor (experimental) alalia is caused by intrauterine organic damage to the cortical speech-motor analyzer. At the same time, the newborn does not have his own speech, but he perfectly perceives the speech of others. It is necessary to distinguish between efferent and afferent expressive alalia.
Efferent motor alalia is diagnosed with abnormalities of the premotor cortex (posterior part of the inferior frontal gyrus, Broca's area). The pathology manifests itself in kinesthetic articulatory apraxia (distortion of the sound of consonants and vowels). During physiological development, the premotor cortex in a child is responsible for the coordination and sequence of movements, which is very important for the formation of speech. Children with efferent alalia find it difficult to repeat a series of movements; they have difficulty reproducing correct articulation. It is with this problem that the phenomenon of persistence is associated: the inability to reproduce syllables in the required order.
Afferent motor alalia develops as a result of lesions in the postcentral zone (parietal parts of the left hemisphere). In healthy children, the postcentral zone is responsible for analyzing sensations at the time of conversation, and the synthesis of a motor program immediately occurs: open the mouth, lower the jaw, inhale air, raise the tongue. With afferent alalia, the child is not able to independently perform a chain of movements to pronounce sounds, so smearing, rearranging or swallowing of sounds occurs. Simply put, the baby has no idea about the sequence of actions of the articulatory apparatus when speaking, and it is difficult for him to reproduce movements even when repeating after his parents. In case of motor alalia with concomitant developmental pathologies, the child is assigned a disability.
Impressive alalia
The main cause of sensory alalia is damage to the auditory-speech analyzer in the cortical region (posterior third of the superior temporal gyrus, Wernicke's center). Patients with this disease have good hearing and developmental abilities. The main problem of correcting pathology is poor memory for pronunciation and a gap in understanding between the sound and meaning of words. The consequence of such dissonance is a lack of contact with others, a distortion of visual perception and a delay in the overall development of the child’s psyche.
Forecast and prevention of ANR
For motor alalia, the prognosis for recovery is always favorable. The result of therapy for sensory and sensorimotor diseases is uncertain and depends on many factors: the degree of damage to the speech center of the brain, side pathologies, and the presence of psychosomatic disorders. At school age, children with ODD are faced with written language disorders: dyslexia and dysgraphia.
Prevention of alalia includes:
- monitoring the course of pregnancy;
- long-term breastfeeding;
- early diagnosis of congenital pathologies;
- complex physical development of the child.
This article is posted for educational purposes only and does not constitute scientific material or professional medical advice.
Diagnosis of alalia
Patients diagnosed with alalia need to be examined by the following specialists:
- Speech therapist - for perinatal history, identifying features of speech and psychomotor underdevelopment, as well as drawing up a model of lexical and grammatical structure, correction of phonemic processes and impressive speech.
- Neurologist - to identify the source of neuralgic dysfunctions and genetic abnormalities.
- Psychologist - to diagnose auditory-verbal memory, timing of psychomotor development, articulatory motor skills.
- Otolaryngologist - when drawing up a therapeutic treatment plan, it is necessary to exclude damage to the function of the hearing aid.
For additional diagnostics and identification of the degree of brain pathologies, the following is carried out:
- EEG;
- otoscopy;
- audiometry;
- MRI of the brain;
- X-ray of the skull;
- echo-encephalography.
Corrective work
Speech therapy correction includes several areas and stages:
- Stimulation of speech activity. At the initial stage, it is important to create motivation, activate speech reactions, teach to imitate someone else’s speech, and enrich the vocabulary. The baby also learns to conduct a dialogue. It is easier to achieve results if you use a game form of training;
- Stimulation of phrasal speech. This stage begins after the baby has formed a certain set of words and develops the skill of conducting a dialogue. Then it becomes possible to construct simple sentences that gradually become more complex. At the same time, children learn the correct construction of words and sentences, grammatical errors disappear from their oral speech;
- The development of coherent speech involves teaching a child how to conduct a monologue or story. He learns to formulate a thought, retell what he read or heard, compose a story based on a picture, and compose. Grammar is reinforced;
- Elimination of phonetic-phonemic disorders through various exercises. The baby learns to pronounce sounds correctly, focusing on the position of the organs of articulation during classes and in everyday life. Over time, such control becomes automatic.
We would like to note the role of parents in the development of speech in a child. It is important to encourage his successes and his speech activity in every possible way. But if something doesn’t work out yet, you shouldn’t scold him.