What is dysarthria
For the first time, people started talking about a speech disorder, which was later called dysarthria, about a hundred years ago. Then the researchers identified a group of sound pronunciation disorders, calling them tongue-tied. A little later it was divided into functional and organic. At the same time, factors that could lead to dysarthric speech disorders were identified.
Despite the fact that dysarthria has been studied for so long, much remains unclear. Today there are two main approaches to the study of this speech disorder:
- neurological. This direction takes into account the clinical manifestations of dysarthria and the area of damage to the central nervous system. Speech disorders are considered in conjunction with other movement disorders that the patient has.
- neurophonetic. Phonemic analysis of dysarthric speech is carried out taking into account psycholinguistic techniques. More attention is paid to identifying and studying neurophonetic syndromes of dysarthria, and the clinical picture of pathology fades into the background.
That is why different researchers give different concepts of pathology. Some people believe that dysarthria should be called a pronunciation disorder in which the prosodic aspect of speech is disrupted. In this case, the definition of pathology is given based on its external manifestations. A number of researchers call dysarthria a coordination disorder of speech that occurs as a result of damage to the efferent system and motor analyzer. That is, unintelligible speech is only a symptom of another pathology.
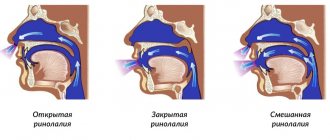
Both of these definitions are correct and in some way complement each other. In simple terms, dysarthria can be called any disorder of sound pronunciation caused by organic damage to the brain. This can be either a complete lack of speech or a nasal, slurred tone of pronunciation.
The controversy extends beyond the definition of dysarthria itself. The classification of the types of this speech dysfunction also causes a lot of controversy.
Symptoms
Dysarthria is a deviation characterized by unclear, incomprehensible, slurred speech due to the fact that the muscles of the soft palate, tongue, larynx, vocal cords, and respiratory muscles function poorly. Defects in the presence of this disease are varied, and many of them overlap with other types of speech disorders, for example, there is a weak, quiet, muffled, nasal voice. Dysarthria is diagnosed based on the following symptoms:
- muscle hypotension;
- muscular dystonia;
- muscle spasticity;
- violations of sound pronunciation - erased dysarthria is characterized by blurred speech, more severe degrees - slow speech, slurring, omission of sounds, distortions, at 4 degrees - absence of speech.
Specific features that manifest dysarthria in children and adults are persistence of defects, learning difficulties, a longer period for automation, violation of both vowels and consonants, interdental and lateral pronunciation of sibilants and sibilants. Illness in children may be accompanied by OHP and dysgraphia.
Types of dysarthria according to O.V. Pravdina
Now there are several principles for dividing speech pathology such as dysarthria into types. In domestic speech therapy, the most common classification is based on the location of the affected part of the central nervous system.
The neurological approach is reflected in the classification proposed by O. V. Pravdina. Their description is presented in the table below:
| Name | CNS affected area | Speech Impairment |
| Cortical | Cortical structures of the brain. It is the cortex that is responsible for the functioning of the speech muscles and the human ability to speak. | Partial paralysis of the muscles of the articulatory apparatus, the sequence of movements when setting articulatory poses is disrupted. The pronunciation of consonants suffers. |
| Subcortical (extrapyramidal) | The striatum and pallidum are subcortical nuclei. These structures regulate muscle tone and also make it possible to give emotional expressiveness to speech. | The muscle tone of the speech apparatus is unstable, the muscles contract involuntarily. The person experiences difficulty trying to maintain articulatory posture. Sound disturbances are unstable. |
| Cerebellar | Conducting pathways and cerebellar nuclei. The respiratory, vocal and articulatory apparatus stop working synchronously. | A person’s speech sounds chanted; this happens involuntarily. Most sounds take on a nasal tone. Speech loses its emotional coloring. |
| Pseudobulbar | Systems responsible for conducting nerve impulses from the cerebral cortex to the nuclei of the medulla oblongata. | Bilateral paralysis of the muscles of the speech apparatus, increased muscle tone, they are practically motionless. Characteristic softening of sounds. Complex and differentiated sounds are affected selectively. |
| Bulbarnaya | Peripheral motor nerve nuclei (brain stem) | Paralysis of the muscles of the speech apparatus (right- or left-sided), the ability to involuntary and voluntary movements is lost. Speech takes on a nasal tone. |
Despite the fact that Pravdina’s classification is used by a large number of specialists, many researchers still consider it inaccurate. Most controversy arises regarding cortical dysarthria. This type of pathology is often regarded as a manifestation of motor aphasia, especially in adults.
Speech therapy examination
In patients with dysarthria, neurologists examine general motor skills using special tests. The patient is asked to complete the following tasks:
- Get dressed, put on your shoes, undress, take off your shoes;
- Walk from corner to corner, waving both arms, stop, sit down, stand on your toes;
- Alternately jump on the right, left and on both legs;
- Raise your arms forward, up, back, down.
In this case, the doctor must record the following indicators:
- Range of movements (full, incomplete);
- Execution accuracy (full, incomplete);
- Independence (full or incomplete, performed with the help of a speech therapist);
- Coordination of movements (correct, incorrect or absent);
- Sense of balance (present or absent);
- Posture (correct or incorrect).
The neurologist analyzes the qualitative state of general motor skills: stiffness, motor tension, disinhibition, increased motor activity.
In order to test fine motor skills, the doctor asks the patient to clench and unclench his fingers into a fist, touch all the fingers of his right and left hands in turn with the tip of his thumb, raise both hands with palms facing him, fingers spread wide. The patient is asked to assemble a mosaic, a pyramid, matches or peas. When the patient performs movements, the doctor notes smoothness, accuracy, violation of the tempo of the movements, failure to perform, presence.
Then the neurologist begins to determine the motility of the articulatory apparatus. Disorders of the mobility of the organs of articulation are directly dependent on the depth of the lesion and the form of dysarthria. Typically, diagnosing severe forms of pseudobulbar dysarthria does not cause difficulties, but determining erased dysarthria is associated with significant difficulties. For this reason, neurologists conduct additional examinations to identify muscle paretics. The patient is offered the following tests:
- Pull out the lips with a “proboscis” (instead, a patient with dysarthria exhibits chaotic movements of the lips);
- Smile (the smile with dysarthria is asymmetrical, the paretic side of the mouth remains almost motionless);
- Make the tongue wide (tendency to narrow it).
With paretic dysarthria, the patient cannot hold the tip of the tongue on the upper lip without the help of the lower lip. Blue discoloration, chaotic twitching of the tip of the tongue, and trembling of its muscles may be observed. In patients with dysarthria, facial expressions may be impaired. They cannot wrinkle their foreheads or puff out their cheeks. Movement disorders are especially pronounced with active contraction of the facial muscles.
Other types of classifications
The French neurologist Tardieu proposed classifying dysarthria according to how well others can understand the dysarthric person’s speech. As a result, he identified four degrees of severity of the violation:
- Only a specialist can identify violations.
- Speech problems are noticeable to others, but speech is understandable.
- Only people from his immediate environment can understand a child.
- There is no speech at all or it is incomprehensible even to the child’s loved ones.
This classification is very clear and convenient. It is often used in their work not only by speech therapists, but also by educators, psychologists, and teachers.
In speech therapy work, the division of dysarthria into types is also often used based on the syndromic approach. In this case, the speech therapist should work together with a neurologist. The doctor determines the leading symptom, and the teacher identifies similar defects in the functioning of the speech apparatus.
Using this approach made it possible to identify the following types of dysarthria:
- spastic-paretic – with the leading syndrome being spastic paralysis;
- spastic-rigid – spastic paralysis and rigidity syndromes;
- hyperkinetic – hyperkinesis;
- ataxic – ataxia;
- spastic-atactic – spastic paralysis and ataxia;
- spastic-hyperkinetic – spastic paralysis and hyperkinesis;
- spastic-atacticohyperkinetic – spastic paralysis, ataxia, hyperkinesis;
- ataxic-hyperkinetic – ataxia and hyperkinesis.
Dysarthria is also divided into types based on the severity of the disorder. In mild forms, speech disorders are minor, often noticeable only when tired. This form is also called erased.
Mild dysarthria has much in common with dyslalia. The only difference is that dysarthric sufferers experience neurological microsymptoms.
The average degree is direct dysarthria (severe), characterized by obvious speech impairments, it becomes slurred, blurred, but generally remains understandable to others.
In severe dysarthria, a person’s speech cannot be understood. If the pronunciation side of speech is impossible, then this form is called anarthria.
Forecast
The prognosis directly depends on the severity of the disease and how quickly therapeutic measures were started. If you follow all the specialist’s recommendations, complete restoration of speech with erased dysarthria is possible, but treatment requires a serious approach. You should not miss classes with a speech therapist or take prescribed medications.
Severe forms of pathology, unfortunately, in almost all cases leave consequences, but they can be minimal if the right treatment is selected. For children with severe speech disorders there are special kindergartens with speech therapy rooms and consultations with highly specialized specialists (neurologist, psychologist, massage therapist).
If the pathology is congenital, it is necessary to take all measures to prevent the progression of dysarthria - avoid injuries, visit a speech therapist, and avoid contact with aggressive substances that can lead to severe intoxication.
Note. It is easier to prevent a disease than to eliminate its negative consequences later. Therefore, measures to prevent dysarthria have an important role in a person’s life.
Reasons for the development of dysarthria
Dysarthria develops as a result of organic damage to the central nervous system. Pathology can occur at different periods of a person’s life. But modern research has shown that in approximately 80% of cases it is congenital. That is, brain damage occurs during the intrauterine period of life.
The main reasons for the development of congenital pathology include:
- Viral and infectious diseases of the mother.
- Kidney failure, as well as pathologies of the heart and vascular system in women.
- Injuries during pregnancy, both physical and psychological.
- Radioactive exposure of a pregnant woman.
- Conflict of Rh factor and mismatch of blood groups between mother and fetus.
- Severe intoxication, including alcohol, nicotine and drugs.
The above factors pose the greatest danger to the fetus in the first three months of pregnancy.
Pathology can also occur at the time of birth. Previously, birth injuries were considered the main factor in the development of dysarthria. However, modern research has made it possible to classify problematic childbirth as secondary factors that aggravate existing pathologies in the fetus. The primary cause can only be considered the unsuccessful use of obstetric aids by medical staff. Brain injuries resulting from medical errors can lead to the development of cerebral palsy and other pathologies.
Impairment of the motor function of the speech apparatus can occur in a child born completely healthy. Dysarthria can occur as a result of a neuroinfection, poisoning (severe intoxication), brain injury, or oncological pathologies of the central nervous system. In adults, dysarthria can be caused by a stroke.
Correction of dysarthria is carried out in two directions at once. First of all, it is necessary to restore the functioning of the central nervous system, as far as the degree of its damage allows. This is done by a neuropathologist. At the same time, a defectologist or speech therapist carries out speech therapy work, which is aimed at normalizing the functioning of the articulatory apparatus.
Prevention
Quite often, parents of children suffering from dysarthria blame themselves. But this speech disorder in many cases develops for reasons beyond a person’s control. No doctor can predict the development of dysarthria in the prenatal period, but a pregnant woman’s compliance with these rules will reduce the risk of developing all kinds of central nervous system pathologies:
- Timely consultation with a doctor and registration. In modern medicine, it is customary to monitor a woman throughout the entire period of pregnancy. With the help of various studies, doctors assess the condition of the fetus, reduce the risks of developing various pathologies, etc. But many women neglect this, turn to specialists late or do not register at all. The development of pathology is difficult to predict, but it can be noticed in time and appropriate measures taken. The sooner this is done, the higher the chance of having a healthy baby.
- Proper nutrition and giving up bad habits. No matter how trivial it may sound, this aspect is very important for the health of not only the expectant mother, but also her baby. In order for the fetus to form correctly, it is necessary to provide the body with a sufficient amount of useful microelements. Taking medications, alcohol-containing drinks and smoking can make unwanted adjustments to the process of formation of vital organs and the central nervous system. It is especially important to monitor your diet during the first trimester of pregnancy.
- Refuse to visit public places for a while, especially during periods of increased incidence of influenza and other infectious diseases.
Avoid stress, spend more time outdoors, try to get as many positive emotions as possible!
To prevent the development of dysarthria in early childhood, it is necessary to provide the child with proper care. Head injuries and all kinds of diseases, especially infectious ones, undermine the baby’s health and negatively affect his development.
Be attentive to yourself and your child, your health is in your hands!
How to recognize dysarthria
Despite the fact that dysarthria is a very complex speech disorder, it can still be corrected, especially if we are talking about an erased form of the disorder.
Dysarthria can be recognized from the first days of a child’s life, and parents should be wary of the following points:
- When breastfeeding, weak nipple latching and sucking reflex may indicate weakness of the muscles of the articulatory apparatus. Milk leaks from the mouth and even the nose;
- The child, later than his peers, begins to hold his head up (5-7 months), try to sit up and crawl (8-11 months), and walk (after 18 months);
- the child develops speech late, sounds are monotonous, articulation is unexpressed;
- increased salivation. The child cannot swallow his own saliva due to flaccid muscles of the tongue, cheeks and lips. The mouth is always open;
- problems with drinking from a cup, chewing food;
- lack of substantive activity. The baby does not show interest in toys, his actions with them are inadequate or inappropriate for his age;
- The baby does not react to loved ones and does not show joy. There is no smiling, walking, or motor activity of the arms and legs.
At a later age, dysarthria may be indicated by disturbances in breathing and speech rhythm.
A child, when talking, pronounces words with different volumes and intonations or in syllables. With dysarthria, a nasal sound appears. Due to the increased tone of the articulatory muscles, the child may get tired during the conversation. In addition to speech disorders, dysarthria also causes motor disorders. The child may grasp objects too strongly or weakly. The grasp reflex may be absent altogether. Spatial and visual and spatial perception are also affected. The child cannot correctly determine the shape and size of an object, for example, when playing with various sorters or pyramids. Difficulties arise when performing physical exercises.
Fine motor skills are especially affected in dysarthric children. It has long been proven that there is a relationship between the ability to perform precise coordinated movements of the hands, the development of speech and mental perception. Insufficiency of the motor part of the brain leads to the fact that it is very difficult for a child to perform pincer grasp with fingers, or it is not performed at all. In erased forms of dysarthric disorder, the development of fine motor skills helps to quickly “launch” speech.
Children who have a history of pathologies associated with the prenatal and birth periods are required to be observed by a pediatric neurologist. The doctor should pay attention to existing problems. If pronounced deviations in the baby’s development are not observed, then he is removed from the register.
Further monitoring of the child's condition is carried out by his parents. When the first alarming symptoms appear, it is better to immediately contact a specialist.
Treatment
Treatment requires an integrated approach, since monotherapy (taking one medication) will not give anything. The main goals of therapeutic measures are speech correction, normalization of speech breathing and elimination of voice disorders. For these purposes, medications, physical therapy (physical therapy), and speech therapy sessions are prescribed.
Drug therapy
Medicines are selected by the doctor depending on the type of pathology. The following pharmacological groups are most often prescribed:
- Nootropics are drugs designed to increase mental abilities and improve memory. Such drugs include Encephabol, Pantocalcin, Picamilon;
- Sedatives (calming) are medications that relieve nervous tension and have an anti-anxiety effect. The most popular are “Persen” and “Novo-passit”;
- Calcium channel blockers - normalize cerebral circulation, the functioning of the vascular system, and reduce the risk of developing oxygen starvation of brain cells. Cinnarizine, Gliatilin and Instenon are considered effective drugs;
- Metabolics - correction of respiratory functions, improvement of metabolism, normalization of cerebral circulation. They are used for various traumatic brain injuries, hypoxia and other pathological conditions. The most commonly prescribed drugs are Cerebrolysate or Actovegin.
Any prescription is made by a doctor after diagnostics and an accurate diagnosis. Self-medication is unacceptable and leads to aggravating consequences.
Classes with a speech therapist
Speech therapy procedures have a beneficial effect on the muscles of the articulatory organs and develop fine motor skills. Individual techniques are developed by a speech therapist depending on the pathological condition. The set of exercises usually includes:
- Articulation and finger gymnastics;
- Exercises to develop voice (orthophony);
- Breathing exercises;
- Correction of speech expressiveness;
- Treatment and correction of written speech disorders;
- Restoring reading abilities.
Physiotherapy
One of the important techniques for dysarthria of any degree. Exercises are performed at home on an ongoing basis. This can be body turns, forward bends, etc. When performing any complex exercise, it is important to breathe correctly. Take a deep breath through your mouth and exhale slowly through your nose. Gymnastics helps normalize metabolic functions, strengthen the body and improve cerebral circulation.
Massage
Speech therapy massage for dysarthria should be done carefully so as not to cause pain to the patient. An individual set of measures is developed by a speech therapist. To improve articulation abilities, experts recommend several massage exercise techniques:
| Massaging area | Methodology |
| Language | Each exercise is performed at least 5-7 times. First you need to stroke your tongue with your index finger. The movement is spiral. In this case, you need to press lightly, without abusing the force of pressure. The second set of exercises is moderate pinching and stroking. Produced from the tip of the tongue to its middle. |
| Lips | The massage is done with two fingers. Movements are spiral and wave-like. First, the upper lip is gently massaged, then the lower lip and the corners of the lips. The final stage is stroking, light pinching and patting. |
| Sky | First, strokes are made with the tongue in the direction from the fangs to the middle of the palate. Then pats are made in the same direction. Completion: stroking the palate with the tongue in wave-like movements. |
During the rehabilitation period, physiotherapy, acupuncture, medicinal baths, and hirudotherapy (leech treatment) are prescribed. An important role in the treatment of dysarthria is played by dolphin therapy, art therapy (clay modeling, drawing therapy, etc.), and sensory therapy. The effectiveness of treatment depends on the correctness of the selected individual therapeutic program.
The specialists at the Yusupov Hospital have the highest medical categories, many years of experience in successfully eliminating pathology, and use only modern equipment. Thanks to this, each patient is provided with qualified assistance and the most effective individual method for treating dysarthria is selected.
Make an appointment
Examination of the articulatory apparatus
The study of the state of the articulatory apparatus includes an examination of its anatomical structure and motor function. First, the doctor observes the patient’s facial muscles at rest. He pays attention to the severity of the nasolabial folds, their symmetry, whether the mouth is open or closed. He looks to see if there is salivation, evaluates the nature of the lip line and the tightness of their closure, and pays attention to whether there are violent movements (hyperkinesis) of the facial muscles.
Then he moves on to examining the organs of the articulatory apparatus. During the examination, the structural features and anatomical defects of the following organs are characterized:
- lips
- Language
- Soft and hard palate
- Zubov
- Jaws
The study of the motor function of the articulatory apparatus is carried out by repeating the required movement many times. To conduct a study of the motor function of the lips, the patient is asked to close his lips, round his lips as when pronouncing the sound “O”, stretch his lips in a “smile”, raise the upper lip up, lower the lower lip down, repeat the pronunciation of the labial sounds b-b-b many times, p-p-p.
The study of the motor function of the jaw is carried out first by demonstration, and then by verbal instructions. The patient is asked to perform the following movements:
- Open your mouth wide, as when pronouncing the sound “a” and close it;
- Move your lower jaw to the left, then to the right;
- Move the lower jaw forward.
The volume and quality of tongue movements are studied using the following tests:
- Place your wide tongue on your upper lip and hold it while counting from 1 to 5;
- Place your wide tongue on your lower lip and hold it while counting from 1 to 5;
- Move the tip of the tongue alternately from the right corner of the mouth to the left corner, touching the lips;
- Protrude the right, then the left cheek with your tongue;
- Stick out your tongue with a “shovel” or “sting.”
To study the motor function of the soft palate, the patient is asked to perform the following steps:
- Open your mouth wide and clearly pronounce the sound “a” (at this moment, the soft palate normally rises);
- With your tongue sticking out between your teeth, puff out your cheeks and blow hard, as if blowing out a candle flame;
- Run the spatula across the soft palate (normally, a gag reflex should appear).
The duration and force of exhalation is checked by asking the patient to play any wind toy instrument (pipe, harmonica, flute) or to blow on a piece of paper or fluff. The speech therapist makes a diagnosis of dysarthria after a comprehensive examination of the patient.