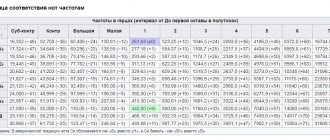
Phonetogram of an 18-year-old patient.
Student of the vocal department of the music school. Soprano. Diagnosis: paresis of the left vocal fold after an acute respiratory illness. The duration of illness is 4 weeks. a - significant narrowing of the frequency range (less than 1 octave, 136.51 Hz) and its shift towards low frequencies. Narrowing of the dynamic range (18.5 dB), shortening of the VMF (11.74 s); b — 1.5 months after electrical stimulation of the larynx and taking neuromidin. Expansion of the vocal profile due to an increase in the frequency (369.02 Hz) and dynamic (38.0 dB) ranges of the voice. Navy - 17.9 s. Unilateral vocal fold paresis (UVP) refers to organic diseases of the larynx, in which the movements of the vocal fold on the affected side are limited or completely absent due to a disorder of the innervation of the muscular apparatus of the organ, which makes it difficult or impossible to regulate vocal function. It is believed that the diagnosis of “paresis” of the larynx can be made if the disease lasts no more than a year, otherwise the diagnosis “paralysis” is more correct [1, 2].
The leading causes of OPGS are tumor processes and surgical interventions on various organs of the neck and chest, most often on the thyroid gland [3-5]. However, in approximately 14% of cases, the disease can be asymptomatic, i.e., without disruption of the vocal and respiratory functions of the larynx [6]. It is interesting that operations performed on the thyroid gland, even in conditions of identification of the recurrent nerve, do not exclude the occurrence of vocal fold paresis. According to T.V. Gotovyakhina [7], the frequency of OPGS during primary surgical interventions on the thyroid gland is 7.5%. Conservative treatment from the first day of the disease ensures restoration of vocal fold mobility in 87.5% of cases. Moreover, the rehabilitation of such patients requires an average of at least 2 months. In cases of delayed therapy for at least 1 month, the effectiveness decreases to 55.5%, for 2-3 months - to 32.7%, for 4-6 months - to 12.2%. When paresis lasts more than 6 months, restoration of laryngeal function, as a rule, does not occur [7].
Diagnosis of vocal fold mobility disorder with paresis, as a rule, is not difficult. In most cases, laryngostroboscopy is used for this purpose. Only 1.7% of otorhinolaryngologists use electromyography in their practice, which is considered the most informative method in the differential diagnosis between paresis and paralysis of the larynx [8].
OPGS significantly reduces the quality of life of patients and often poses a threat to professional fitness. Therefore, the development of new methods of conservative and surgical treatment of the disease still remains relevant. One of the latest achievements in this direction is work devoted to the surgical reinnervation of the vocal laryngeal muscle by implantation of a pedunculated neuromuscular flap through the window of the thyroid cartilage and medial displacement of the arytenoid cartilage. Such operations allow you to restore the tone and vibration of the vocal fold on the side of the paresis with good results. However, this approach is not applicable in the early period of the disease, and is recommended only after 6 months of unsuccessful conservative treatment [9]. In this regard, a significant role in the rehabilitation of the vocal and respiratory functions of the larynx in OPGS is given to stimulating therapy, which consists of activating regenerative processes, cross and residual innervation of the laryngeal muscles and compensatory mechanisms that allow achieving the most complete closure of the vocal folds during phonation, as well as preventing atrophy of the muscular apparatus of the larynx.
The purpose of our study is to optimize the conservative treatment of patients with OPGS.
Patients and methods
The study was conducted at the clinical base of the Department of Otorhinolaryngology of the State Budgetary Educational Institution of Higher Professional Education of the Yaroslavl State Medical University and at the Avicenna Medical Center LLC, Yaroslavl. 50 patients with laryngeal paresis were examined: 45 women and 5 men from 18 to 70 years old. Criteria for inclusion in the study:
age over 18 years, unilateral impairment of laryngeal mobility, disease duration no more than 6 months.
Exclusion criteria:
the presence of contraindications for electrical stimulation of the larynx and the prescription of the cholinergic drug Neuromidin (ipidacrine, Olainfarm JSC), which formed the basis of complex therapy for patients with OPGS. These criteria were: individual intolerance to the drug, peptic ulcer of the stomach and duodenum, severe pathology of the liver and kidneys, exacerbation of bronchial asthma, angina pectoris, bradycardia, mechanical obstruction of the gastrointestinal tract and urinary tract, the presence of episodes of convulsive syndrome, cardiac or other implanted electrical stimulators , metal prostheses in the neck and head, malignant neoplasms of any location, previous surgery for thyroid cancer within 5 years, damage to areas of the skin that will be exposed during electrical stimulation of the laryngeal muscles, pregnancy and lactation.
The leading etiological factor in the development of OPGS was surgery on the thyroid gland, performed for various pathologies: diffuse goiter, nodular goiter, autoimmune thyroiditis. There were 39 such patients (78%). The scope of surgical intervention varied: from partial resection - thyroidotomy to complete removal of the organ - thyroidectomy. In 5 (10%) patients, OPGS developed due to a viral infection. In 6 (12%) cases, the cause of the disease could not be established, so the process was considered idiopathic. The average duration of the disease was 1.9±0.7 months. The earliest request for specialized medical care was 3 weeks after the development of OPGS, the latest was 5 months 12 days.
The degree of damage to the innervation of the muscular apparatus of the larynx was determined using the vocaSTIM-Master device (Physiomed, Germany), which makes it possible to estimate the so-called accommodation coefficient (α), which is the ratio of two threshold values: the galvanic threshold of tetanic contraction of the laryngeal muscles under the influence of triangular currents to rheobase obtained under the action of rectangular currents. Normally, α ranges from 3 to 6. A value below 3 indicates a decrease in the accommodative ability of the laryngeal muscles and the beginning of their denervation (paresis). A coefficient α of 1 and below means a complete loss of the accommodative ability of the laryngeal muscles, which indicates the presence of paralysis. Patients with an α level greater than 1 were included in the study.
By randomization, patients were combined into two groups, A and B, 25 people in each. The groups were statistically comparable in terms of age and gender, etiological factors, clinical and functional characteristics, as well as the duration of the disease (Levene Test: p
>0.05). In both groups, complex treatment was used, including breathing exercises, training of the external neck muscles, vitamin therapy, neuromuscular electrophonopedic stimulation (NMEPS) of the larynx and standard voice exercises, which the patient, after preliminary training, performed daily at home.
In group A, treatment was supplemented by the administration of the cholinergic drug neuromidin, which has a stimulating effect on the conduction of impulses along nerve fibers, interneuronal and neuromuscular synapses of the central and peripheral nervous system. The pharmacological action of the drug is based on a combination of two mechanisms of action: blockade of potassium channels in the membrane of neurons and muscle cells and reversible inhibition of cholinesterase in synapses, due to which neuromidin not only improves impulse conduction in the nervous system, but also increases the contractility of smooth muscles. In addition, neuromidin has nootropic, mnemotropic and psychostimulating effects. The latter is quite important for patients suffering from laryngeal paresis, since loss of voice sonority significantly affects their quality of life. According to modern evidence-based research, neuromidin activates adaptive neuroplasticity [10], which accelerates the processes of recovery of lesions of the nervous system of various locations. Neuromidin activates recovery processes in both the central and peripheral nervous systems - this is its fundamental difference from other anticholinesterase drugs. This property of the drug allows one to maintain the activity of projection zones in the central nervous system in case of damage to peripheral innervation, which increases the effectiveness of therapy. Neuromidin was prescribed for the first 10 days as intramuscular injections of 15 mg once a day, then switched to oral administration at a dosage of 1 tablet (20 mg) 3 times a day. The total course of treatment was 45 days. Neuromidin was not used in group B patients.
Electrical stimulation of the larynx in both groups was carried out using the vocaSTIM-Master device operating in low and medium frequency pulsed current modes. The supply of currents to the laryngeal muscles was carried out using a hand key by the patient himself. The treatment method is a combination of contractions of the laryngeal muscles under the influence of pulsed currents in response to the patient’s simultaneous performance of phonopedic exercises, which were selected for each patient individually according to the coefficient α. The NMEFS course consisted of 40 sessions, 2 sessions per day for 20 days. After this period, the patients performed a set of phonopedic exercises independently.
The results of therapy were assessed after 45 days. Full restoration of vocal fold mobility was assessed as “recovery.” Restoring voice sonority while maintaining the visual picture of paresis was characterized as “improvement.” Maintaining the immobility of the vocal fold and dysphonia at the same level was recognized as “no effect.” The criteria for the analysis were methods adopted as standards in modern otorhinolaryngology and phoniatrics and allowing to assess the clinical and functional state of the larynx. Optical laryngostroboscopy was used to determine the mobility of the vocal folds, their vibrator activity, and the degree of closure during phonation. The dynamics of the respiratory function of the larynx was studied by screening flowmetry using a portable flow meter ATS 97 with recording of forced inspiratory volume (FEV) in l/min. Laryngeal vocal function was studied using the GRBAS scale, subjective listening to the patient's voice by three independent experts and acoustic voice analysis.
Voice assessment on the GRBAS scale was carried out according to five standard criteria: “grade” (G) - severity of dysphonia, “roughness” ® - roughness, harshness of the voice, “breathiness” (B) - breathing disorder, presence of shortness of breath, aspiration, “asthemicity” ( A) - weakness of the voice, “strain” (S) - tension of the voice. Each criterion was determined in points from 0 to 3, where 0 is normal, 1 is mild symptom severity, 2 is moderate manifestation, 3 is strongly expressed symptom. Acoustic analysis was carried out using computer software “The lingWAVES Phonetogram Pro” (ATMOS, Germany) with a phonetogram recorded. In this case, the following indicators were subject to evaluation: time of maximum phonation (TMP), instability (perturbation) of the fundamental tone (Jitter), frequency and dynamic ranges, loud voice intensity, dysphonia Severity Index (DSI). In addition, the patients' quality of life was assessed. For this purpose, the specialized Voice Handicap Index (VHI) questionnaire was used in its full version. All studies were carried out twice: before the start of treatment and after 45 days of therapy.
Statistical analysis of the obtained data was carried out using Statistica version 10. When comparing groups A and B, differences were considered significant if the obtained p
for the compared criterion was below the critical significance level α=0.05. The compared characteristics were classified as quantitative. To evaluate them and test statistical hypotheses, we used an analysis of the correspondence of the type of distribution of attribute values to the law of normal distribution using the Shapiro-Wilk test, descriptive statistics, a two-sided test for independent variables, Levene’s test for homogeneity of variances, and parametric analysis of variations.
Vocal cord care
Acupressure performed early in the morning will invigorate the body and tune the speech apparatus to the desired wave. To properly restore the vocal cords, you need to fully concentrate on the massage. This will help identify areas where there is obvious discomfort, any kind of pain or tingling sensations.
They should be handled with special care. You need to massage clockwise, repeating circular movements at least 8 times. Sensitive points on the temples and at the wings of the nose, on the chin and behind the ears, on the neck and between the eyebrows will help both improve the vocal cords and increase overall tone. Chanting is another good answer to the question of how to develop your vocal cords. If you feel that working with diction alone is not enough to achieve the desired level of oratory skills, then try adding the basics of acting to your arsenal. This can be done either by signing up for courses or by participating in extras or casting.
Share this article:
I liked the article
Results and discussion
The main complaints of patients before the start of therapy were voice timbre disorder in the form of hoarseness, increasing after vocal stress (90% of observations) or aphonia (10%), coughing (100%), shortness of breath when talking (72%) and/or during physical activity ( 94%), choking while eating liquid or solid food (34%). The severity of symptoms was determined by limited mobility and vibrator activity of the vocal fold on the affected side (3 patients in group A and 4 patients in group B) or complete immobility of the fold during phonation (22 and 21 patients, respectively), which was confirmed by stroboscopy data. In most cases (90%), the vocal fold on the affected side was in the paramedian position (22 observations in group A and 23 in group B). Only 10% of patients (3 from group A and two from group B) had a lateral location of the fold, which caused aphonia, created additional difficulties in therapy and worsened the prognosis of the disease.
The study proved that adding the cholinergic drug Neuromidin to the treatment regimen for OPGS allows one to achieve better results. Thus, in group A, recovery occurred in 5 patients (20%), improvement in 17 (68%), and there was no effect in 3 cases (12%). In group B, recovery occurred in only 2 patients (8%), improvement in 16 (64%), and no effect in 7 (28%). Thus, the overall effectiveness of complex treatment of patients in group A was 88%, in group B - 72%. The differences between the groups are statistically significant in two assessment parameters: “recovery” and “no effect” ( p
<0,05).
The data presented above were confirmed based on an analysis of the dynamics of the compared parameters of the state of the respiratory function of the larynx, voice and quality of life of patients. It was noted that FEV before treatment was significantly reduced in both groups: in group A - 147.2±32.0 l/min, in group B - 152.6±37.9 l/min. During the treatment, there was a positive dynamics of the indicator, but in group A, FEV increased to 288.7 ± 37.7 l/min, i.e., almost 2 times, and in group B, the increase in FEV on average did not exceed 45 l/min and amounted to 197.2±34.5 l/min. The differences between the groups are statistically significant, p
<0,05.
Before treatment, the GRBAS score was 8.4±1.2 points in group A and 8.3±1.7 points in group B, after treatment - 4.1±0.6 and 5.9±0.7 points, respectively ( R
<0.05).
It was found that in group A, compared to group B, there was a more pronounced dynamics of almost all acoustic parameters of the voice. Thus, the initial value of VMF in group A was 5.2±1.4 s, after treatment - 11.6±1.7 s. In group B, IMF increased from 6.0±1.6 s to 9.1±0.6 s. In group A, there was a doubling of the frequency range, from 128.1±37.3 Hz to 275.3±46.7 Hz, and the dynamic range - from 14.0±2.3 dB to 24.0±2.7 dB ( p
<0.05).
In group B, the dynamics of indicators were not so noticeable. The frequency range increased from 139.0±26.3 Hz to 195.3±22.6 Hz, the dynamic range - from 14.9±1.9 dB to 19.0±1.3 dB. In group A, the rate of voice instability in frequency decreased threefold, from 3.4±1.5% to 1.0±0.3%. In group B, Jitter remained quite high, from 3.2±1.8% it decreased to only 2.9±0.3%, which explained the persistence of tremolation and diplophony in the patients’ voice. The change in the acoustic parameters presented above was accompanied by a shift in the dysphonia index towards positive values. However, in group B these changes were not so noticeable (from –2.9±2.3 to –0.1±1.4) compared to group A (–3.0±1.7 to –1.9 ±2.3). The differences between the groups are statistically significant, p
<0.05.
However, it should be noted that there were no significant differences between the groups for a number of parameters. Thus, in patients of group A, the loud voice strength increased from 74.0±4.5 dB to 85.8±6.9 dB, in group B - from 75.8±6.6 dB to 84.7±5, 5 dB( r
>0.05).
At the same time, the average values of the indicator were quite satisfactory in both groups and corresponded to the age norm. The dynamics of the quality of life indicator also did not have significant differences between the groups. In group A, VHI before treatment was 84.9±12.6 points, after treatment - 27.0±9.6 points. In group B, VHI decreased from 81.0±20.2 to 32.1±11.7 points ( p
>0.05). In general, in both groups compared, VHI did not correspond to normal values, which indicated that the quality of life disorder persisted in the majority of patients.
In the pictures
phonetograms of a patient from group A are presented. The dynamics of the vocal profile clearly demonstrates the effectiveness of complex treatment of OPGS. In this observation, complete restoration of vocal fold mobility on the affected side was achieved.
An analysis of all cases of ineffectiveness of the therapy, as well as patient dissatisfaction with respect to the dynamics of vocal function, suggested that possible reasons for the lack of effect are the patients’ late seeking of medical help (after 2 months or more), the lateral location of the vocal fold on the affected side, as well as failure by the patient to comply with recommendations on the advisability of systematically performing phonopedic exercises.
It should be noted that the majority of patients in group A tolerated neuromidin satisfactorily, despite the long course of therapy. Side effects and adverse events were recorded in only 2 (8%) cases out of 25. One patient, a 67-year-old woman, complained of weakness and hand tremors after switching from the injection form of Neuromidin to the tablet form. The symptoms disappeared within 24 hours without stopping the drug. The second patient, a 46-year-old woman, noted frequent headaches throughout the entire period of neuromidin therapy. In this case, discontinuation of the drug was also not required.
DIAGNOSTICS
When diagnosing dysphonia, it is necessary to consult such specialists as a pediatrician, endocrinologist, pediatric surgeon, otolaryngologist, and speech therapist.
First of all, the following is carried out:
- Physical examination of the child and collection of anamnesis (a set of data obtained by interviewing the subject). A visual examination of the larynx is performed, through which it is possible to assess the condition of the mucous membranes of the larynx and the functionality of the vocal folds.
- Acoustic voice research. The frequency and amplitude of the voice while reading is measured.
- Laboratory diagnostics. Collection of general tests: blood, urine, biochemical blood test.
- Examination by an otolaryngologist. An examination is performed for velopharyngeal insufficiency and assessment of airflow through the airways.
- Speech therapy examination of a child with dysphonia. The speech therapist evaluates the medical history; clarifies what complaints there are; studies the nature of voice formation and vocal attack; examines physiological and phonation breathing; checks tempo-rhythmic and intonation parameters of speech.
conclusions
Laryngeal paresis is a common complication that occurs after various diseases and surgical interventions. OPGS is characterized by significant disturbances in all acoustic characteristics of the voice, which certainly affects the quality of life of patients and their communication abilities.
The data obtained during the study indicate the advisability of complex therapy for OPGS, which is a combination of electrical stimulation of the larynx, phonopedia and the prescription of cholinergic drugs. The addition of neuromidin to the generally accepted conservative treatment regimen can increase its effectiveness from 72 to 88%.
In conclusion, it should be emphasized that in cases of development of OPGS, a correct attitude towards the patient, maximum effort, perseverance and professionalism is necessary to restore laryngeal function or, at least, improve voice quality.
Massage for dysarthria
The mechanism of action of massage is complex. It consists not only of a direct mechanical effect on the tissue being massaged, but also of a neuroreflex and humoral effect. In speech therapy work for dysarthria, it is necessary to skillfully use massage techniques, both relaxing tense spastic muscle groups and leading to irritation and toning of the neuromuscular speech apparatus.
To best obtain the relaxation effect, you need to create a calm environment: the room should be warm, the child should not be distracted by anything, he should sit or lie comfortably, without tension and not focus his attention on the organs of the speech apparatus - all this can be achieved with the help of autogenic training and some other psychotherapeutic techniques. You can turn on soothing music or an educational cartoon.
The massage should be carried out with warm, dry hands wearing gloves, using light strokes necessary for a specific muscle group. With a tonic massage, on the contrary, more intense and sharp movements of kneading, patting, and tapping are recommended. Massage of the affected muscle group should be preceded by an impact on the entire neck-brachial area to enhance blood and lymph circulation. When using probe massage, instruments must be thoroughly washed and sterilized in a special solution.
To achieve the best result of correctional work, it is advisable to combine massage with exercises of passive and active articulatory gymnastics, which allow you to teach the child to relax all spastic muscles, achieve the full amplitude of voluntary movements, hold the lips and tongue in a certain position, inhibit synkinesis, achieve precision in articulatory postures and switch easily from one articulatory pose to another.
As a rule, sets of exercises are selected individually, taking into account the clinical manifestations of dysarthria, the degree of its severity, the child’s age, his personality, intelligence, etc. In all cases, breathing exercises are included in the set of exercises for speech therapy correction, since breathing is the energetic basis of speech and in case of weak Speech breathing makes it difficult to form both the voice and speech noises.