- home
- Services and prices
- Neurology
- Restoring speech after a stroke
A stroke is an acute disruption of the blood supply to the brain, when cells in the nerve centers die from a lack of oxygen and neural connections are destroyed. Its consequences can be very different: memory loss, partial or complete paralysis, dementia and speech disorders. The latter are classified into several types: light, medium and heavy.
However, the results of a stroke are not irreversible: in most cases, it is possible to return the victim to normal life with the help of a set of rehabilitation measures.
Signs of speech impairment
The fact that the areas of the brain responsible for speech were damaged during a stroke is indicated by the behavior of the victim:
- The patient confuses words and sounds, stumbles, stutters;
- The construction of sentences is disrupted - instead of “I went to the street,” a person can say “I went to the street,” etc.;
- Frequent repetition of the same sounds or words;
- The patient does not understand well what is being said to him, forgets the names of objects;
- Consistent counting skills are impaired;
- Obscene words and expressions appeared.
The last factor often comes as a surprise, since after a stroke even cultured and well-mannered people can begin to swear. Experts say that this is due to the ancient origin of obscene language.
Types of speech disorders
Modern medicine knows two main types of speech disorders after a stroke: aphasia and dysarthria. In the first case, speech is impaired due to the death of neurons and their connections in the brain center that is responsible for speech. Aphasia can be complete or partial. Dysarthria occurs against the background of the fact that the centers in the brain responsible for the functioning of speech muscles have been damaged.
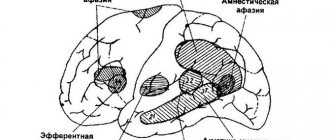
Aphasia
It is the most common cause of speech impairment. There are six variations of aphasia in total:
- Motor
. This form is divided into two more types of aphasia. With afferent aphasia, the patient cannot choose the articulatory posture that is needed in order to pronounce specific sounds. With efferent aphasia, speech is preserved at an instinctive level, but repetition is impaired. Victims have difficulty moving from one position to another. - Dynamic
. In this variant, patients experience problems with active utterance: the inability to correctly formulate a sentence because both external and internal speech are impaired. There are frequent cases of echopraxia - repetition - situations when the patient automatically begins to repeat words, phrases, facial expressions or gestures after the interlocutor. - Sensory
. It is divided into three types: cortical, subcortical and transcortical aphasia. In the first case, the patient lacks both understanding and pronunciation of sounds; in the second, the transmission of impulses from the parts of the brain responsible for the perception of sound information is distorted. In the third case, writing and visual function are impaired, but the patient is capable of perceiving light speech structures. - Sematic
. The victims do not fully understand the complex speech structures that are responsible for spatial relationships. Problems are often observed when completing tasks that contain complex syntactic formulations. Patients forget the names of the simplest household items - dishes, furniture, clothing, electrical appliances, and read slowly. Sometimes acalculia develops, a neuropsychological disease when a person loses the ability to count consistently. - Acoustic-mnestic
. With this aphasia, patients experience difficulties that are associated with the ability to retain information perceived auditorily in memory. During classes with a speech therapist, patients cannot repeat the simplest connections of several words, or understand the meaning of a sentence when it is pronounced at a fast pace or during a conversation with several interlocutors. - Total
. A distinctive feature of this type of aphasia is the complete absence of speech due to damage to a large number of areas of the brain. Total aphasia is subject to hard and long-term correction work from various specialists - from massage therapists to speech therapists.
Dysarthria
A type of speech disorder when a stroke victim has impaired functioning of the organs responsible for articulation (tongue, palate, lips). It is observed much less frequently than aphasia and develops, as a rule, with damage to various brain structures, in particular the cranial nerves involved in the work of speech muscles. Patients experience sluggish and uncertain speech, and difficulty pronouncing individual sounds or words.
Articulatory dyspraxia
Another type of speech impairment is the inability of a person to make consistent movements with the mouth, lips, and tongue - which is divided into two types: kinetic and kinesthetic.
In the first option, difficulties arise when sequentially changing sounds and syllables, skipping them, replacing one syllable or sound with another, and incorrect placement of stresses.
In the second option, disturbances occur in the articulatory structure: the brain experiences difficulty interacting with the muscles responsible for producing sounds.
The formation of motor skills is carried out through adequately coordinated actions. After a stroke, neuronal death can occur in areas of the brain with the premotor, profrontal and motor cortices, which can lead to dyspraxia.
The correction of dyspraxia is carried out by a speech therapist in collaboration with a neurologist and psychologist.
General rules of care
The recovery period after a stroke is divided into early (up to 6 months), late (6-12 months) and residual effects (after 1 year). Ideally, in the early recovery period, the patient is recommended to be treated in palliative hospitals, sanatoriums, in the late recovery period and during the period of residual effects - in a day hospital, rehabilitation department, or by a visiting team at home. In reality, most often patients are at home after an acute period of stroke, and the main question that arises among their loved ones is where to begin rehabilitation. One of the main tasks of the rehabilitation process is to create comfortable conditions that promote relief and speedy recovery.
Preparing the premises
To exclude the impact of external traumatic factors (light, sound, temperature stimuli) on the patient’s psyche, he should be placed in a bright, well-ventilated room, where no extraneous noise can be heard from the street. The room should maintain a comfortable temperature within +18-22 °C.
The room should not be cluttered with furniture or objects that are easily moved out of place. A good alternative to a regular bed would be a functional one - with adjustable height and backrest position, side rails, and lockable wheels. Near the bed you need to place a bedside table with hygiene items, a blood pressure monitor, other necessary things, a wheelchair or other mobility aids (walkers, canes), a portable toilet or a bedpan.
If the person caring for the patient is not always with him, you can equip the room with a call button that the patient can easily reach, or replace it with a regular bell. Patients who can move independently or are beginning to train the skill of walking will find handrails along the walls very useful, and anti-slip mats in the bathroom will prevent injuries.
Body hygiene and bedsore prevention
Adequate prevention of bedsores can prevent their occurrence in 80% of cases.
Preventive measures:
- a special anti-bedsore or foam mattress with a thickness of at least 10 cm;
- soft bed linen without wrinkles;
- special cushions or pads made of foam rubber for vulnerable parts of the body (back of the head, shoulder blades, elbows, sacrum, heels, ankles);
- changing body position every 2-3 hours;
- comfortable underwear;
- prevention of skin trauma - carefully moving or turning over the patient.
It is important to carry out proper hygiene measures and skin care. At least once a day, during hygienic procedures, you should examine the entire surface of the patient’s body, vulnerable areas - every time you turn over. You should use waterproof diapers and diapers and change them as needed. It is necessary to wash the patient with warm water without soap after each bowel movement, washing with soap - no more than once a day, it is better to use liquid soap. After washing, the skin is thoroughly dried with a soft towel. For dry skin, moisturizing and nourishing creams are used; for diaper rash, powders without talc are used.
Nutrition
Food should be comfortable to swallow and easily digestible. The patient needs a sufficient amount of fluid - at least 1.5 liters. in the absence of restrictions. Drinking should not be limited even with urinary incontinence, since with a lack of fluid, urine becomes concentrated and irritates the skin.
The patient's diet should contain a sufficient amount of protein. It can be a soufflé, minced chicken, beef, rabbit, or fish. Patients who have difficulty chewing or swallowing semi-solid foods may be given meat or fish broth.
The menu should include dishes rich in vitamin C, iron, zinc, fermented milk products, fruits and vegetables.
Food is prepared boiled or baked and must be freshly prepared. You should not eat fried foods, pickles, smoked foods, spicy foods, canned food, fast food, carbonated and sweet drinks. You need to eat 4-5 times a day, in small portions.
Ways to restore speech after a stroke
Speech after a stroke is rehabilitated through a set of various measures. This includes taking medications that improve blood circulation and promotes the formation of new neural connections, and physical therapy, massage, speech therapy and articulation exercises, and much more. A plan for speech restoration after a stroke for a particular patient is developed individually based on research and the diagnosis made. Some aspects of rehabilitation therapy require specialist supervision, but not all of them. The patient can perform some exercises to restore speech after a stroke with the help and participation of people close to him, which will make the recovery process more effective.
As soon as the patient's condition has stabilized, the very first exercises begin. The patient is examined by a speech therapist and a neurologist. Special tests help identify existing problems and prescribe further treatment.
There are no guarantees that a person will fully restore speech skills: much depends on how severe the brain damage was, on the body’s ability to regenerate and the interest of the patient and his loved ones in achieving the goal.
It is strictly not recommended to self-medicate and teach the patient to talk on his own. There is a risk of developing complications in the form of echolalia - meaningless repetition of words, verbal embolus, agrammatism, etc. A set of treatment measures is prescribed exclusively by a group of treating specialists.
Speech therapy exercises
Regular sessions with a speech therapist are the key to speech restoration. At first, the specialist works with the patient himself, then relatives can continue training at home.
The basis of a speech therapist’s work is the involvement of certain parts of the brain in the control of speech functions. To do this, he uses different techniques and sets of exercises:
- Phonetic. Through the victim repeating individual sounds, words and phrases after the doctor, the type of speech disorder is determined. The facial muscles of the tongue and lips are under control.
- Semantic. The active thought process is stimulated. A person who has suffered a stroke must complete sentences, series of associations, and talk on various topics.
- Visual. The use of cards with images, book illustrations and other specialized items so that the patient begins to build various connections and associative series. This method is usually used for sensory aphasia.
- Creative. Various types of creative activities are included in the rehabilitation work, in particular those that the patient was interested in. This could be expressive reading of tongue twisters, poetry, acting, music, singing, drawing, etc.
There are several rules for completing tasks:
- Gradually increasing the complexity of the exercises;
- Encouragement of the patient's achievements is mandatory;
- Monitor the patient’s condition and prevent overwork;
- Number of classes – no more than 5-10 per week.
Based on the patient’s progress, the speech therapist should adjust the rehabilitation program from time to time.
Massage
After a stroke, there are often cases of not only speech impairment, but also the appearance of problems with the speech apparatus: in patients, chewing function is impaired, uncontrolled salivation appears, and the corners of the mouth and cheeks sag. There is a need to restore muscle tone and start the process of restoring correct facial expressions. Here a special massage comes to the aid of the patient, which is prescribed by the attending physician depending on the characteristics of the injury in a particular person.
The main objectives of massage within the framework of rehabilitation therapy are:
- Improving blood circulation and activating lymph outflow;
- Normalizing the tone and elasticity of muscle tissue;
- Strengthening the general condition of the body;
- Relieving tension and anxiety in patients.
Massage is prescribed almost immediately after the patient’s condition has stabilized: approximately one to two weeks after the crisis. At first, these are simple stroking of the muscles and gentle rubbing at a moderate rhythm. Then the techniques become more complex, kneading and vibration are used, the intensity and duration of the sessions increases.
The decision to prescribe or refuse massage courses is made by the attending physician. Sometimes a patient may have contraindications to it, an increased risk of developing severe deviations from the norm of body functionality, and other complications.
Articulation exercises
This type of exercise is used to increase control over the muscles involved in speaking.
Speech therapy exercises that develop language:
- Stick it out and hold it in this position for a few seconds;
- Try to reach your nose with your tongue and hold it;
- Pass it from one corner of the mouth to the other several times;
- Move your tongue back and forth across the palate;
- Clatter;
- Lightly bite your tongue after relaxing it;
- Trace your lips first counterclockwise and then clockwise.
Exercises to develop lips:
- Fold them into a tube and pull them out;
- Smile with your mouth closed;
- Raise your lip up, showing the upper row of teeth;
- Roll the air in different directions, inflating first one or the other cheek;
- Blow through your lips, having previously relaxed them;
- Use your fingers to pull them up, down, right, left;
- Alternate between raised and lowered corners of the mouth.
Exercises to restore your voice:
- Alternate pronunciation of vowels;
- Silent articulation of “Y”;
- Pronunciation of vowels one after another with a smooth transition of sound, while reversing stress;
- Repetition of consonant sounds - from voiceless to voiced.
Exercises for facial expressions:
- Working with eyebrows: frowning, being surprised with their help;
- Open very wide and then relax your mouth;
- “Kiss” the air;
- Stick your tongue out to your interlocutor and pull him in different directions;
- Move your jaw.
Depending on the type of disease, the doctor selects an individual set of tasks for each patient.
Breathing exercises
Classes with a speech therapist will be many times more effective if, before starting speech exercises, you perform physical exercises that will improve articulation and function of the facial muscles:
- Pull the letter “U” through the elongated “tube” lips;
- Smile several times so that symmetry is maintained at the corners of the lips;
- If the loss of sensitivity is insignificant, slightly bite the lower and then the upper lip;
- Roll up your tongue;
- Smack expressively;
- Run your tongue over your lips and palate;
- Calmly inflate and deflate your cheeks.
To achieve positive dynamics, exercises must be performed regularly.
Drug therapy
Taking medications in the post-stroke period allows you to prevent the process of cell destruction, normalize blood circulation and start the process of tissue regeneration.
Experts prescribe different types of drugs:
- Blood thinners – medications that reduce blood viscosity and stimulate improved blood circulation;
- Diuretics – relieve swelling, including in the brain;
- Nootropic drugs – stimulate the regeneration of nerve cells;
- Antihypertensive drugs – do not allow blood pressure to reach a critical value, which can cause complications.
Music therapy
In certain situations, when the patient does not speak at all, but can sing, treatment with music helps. All exercises with a speech therapist in such a situation involve singing: the patient sings sounds, words, sentences, repeats the words and motive after his favorite performer.
In addition, music has a positive effect on the human psyche, calming or making him happy. Often patients are in a state of depression or increased anxiety, and here music comes to the aid of specialists, which stabilizes the emotional background.
The positive effect of music on brain recovery after a stroke was studied in scientific workshops. During classes, people with speech impairments had their cerebral cortex activity measured. It has been proven that music stimulates the functioning of the nervous system, promotes the formation of new neural connections, and therefore restores brain properties lost during the disease.
Physiotherapy
A set of therapeutic practices and techniques for stimulating the articulatory apparatus and vocal cords by exposure to electrical impulses, magnetic radiation, light, heat or air, ultrasound, etc.
Some of the main goals of physiotherapy after a stroke are:
- Prevention of complications and new stroke;
- Improving blood circulation and metabolism;
- Preventing the occurrence of blood clots, which can lead to blockage of blood vessels;
- Restoration of muscle tone;
- Relieving pain and swelling;
- Improving the passage of nerve impulses, accelerating the formation of new neurons;
- Normalization of sleep patterns and general well-being of the patient.
Acupuncture
A popular procedure is used to correct motor aphasia and helps restore the tone of the speech apparatus.
The effectiveness of acupuncture has long been proven by science: needles irritate nerve endings in the skin, send signals to the brain and spinal cord, thereby activating the central nervous system and promoting the formation of new neurons. Also, when using this method, muscle activity improves, pain decreases, and the immune system is activated.
Traditional methods
Treatment of stroke with herbs is sometimes practiced by some doctors, prescribing it as an auxiliary therapy. Taking decoctions of viburnum, thyme, St. John's wort, rose hips, and calendula, of course, can help improve blood circulation or increase the body's overall resistance, but it is not a panacea.
We do not recommend starting treatment of relatives who have suffered from a stroke on their own using traditional methods: first consult with your doctor and make sure that the patient is not allergic to this or that drug.
Speech Pathologist Tips and Tricks
Dealing with an emotionally depressed patient is very difficult. Imagine a situation where a person regains consciousness, but he realizes with horror that he is unable to say anything and cannot communicate with others. In this case, “faster” does not mean “better.” The patient should feel the unobtrusive attention of others.
Some tips for relatives:
- Do not treat the patient as an inferior person doomed to disability. Talk to him calmly and carefully. Try to set yourself up for recovery. Pay attention to the smallest positive changes.
- Do not allow indifferent people to approach him. All emotions should be good.
- Play soft music, the patient's favorite radio station.
- Try to interest the patient in a dialogue with you, emphasize the importance of his opinion.
- The hearing load at the patient's location must be controlled. Radio and TV should not be played for long periods of time or loudly. Excessive noise is annoying and tiring.
How long does it take to restore speech after a stroke?
The rehabilitation process usually takes from several months to several years - it all depends on whether the speech centers were severely damaged. Common disturbances in aphasia disappear on average 3-6 months after the crisis.
If the stroke was suffered in a severe form, then the possibility of restoring lost speech skills is about 55%. With moderate severity, it is guaranteed that 75% of the damage can be restored, with mild damage – up to 90%.
The most favorable prognosis is observed in patients who have suffered motor aphasia. In young people, speech is restored almost completely; in older people, minor impairments may remain in the form of unclear pronunciation of individual sounds.
Where is the best place to go for rehabilitation?
The very first actions to regain lost skills begin in a hospital setting. The attending physician develops a treatment strategy and prescribes medications that help accelerate the regeneration of brain cells.
Speech restoration after a stroke is carried out both at home and in special rehabilitation centers in Moscow, where qualified speech therapists-aphasiologists, neurologists, psychologists, and massage therapists work with victims.
The patient is first examined and, based on the diagnostic results, a rehabilitation program is prescribed, which allows the person to gradually return to a normal, fulfilling life. Individual consultations are held with the patient’s family and friends and sets of exercises are prescribed, which will need to be continued to be practiced at home.
Memory training
Memory and intellectual function training occurs simultaneously with speech restoration. The patient should try to repeat the syllables, words, phrases spoken by the assistant, gradually increasing the interval between pronouncing the word and repetition.
Board games, composing stories based on pictures, solving crossword puzzles, and even simple conversations help restore thinking abilities. Near each item in the room you can put a card with its name. As cognitive functions are restored, the patient can read, watch films, and discuss their content.